EHR Adoption: Best Practices for Healthcare Providers (2024)

Since the 1980s, when electronic health records went mainstream, they’ve seen massive adoption in developed economies. Most hospitals in countries like Australia (92%), New Zealand (97%), the United Kingdom (97%), and the Netherlands (98%) are being run electronically.
But, for all they offer, 75% of medical professionals surveyed felt they’d benefit from additional training.
For any new system implemented, a robust user adoption strategy is required to ensure that employees learn how it works, adopt all its features, and use it consistently in their day-to-day workflow.
What Is EHR Adoption?
EHR adoption generally refers to digital adoption, but in this case, it concerns healthcare organizations making an electronic health system part of their day-to-day workflow. It is defined as the process medical firms undergo as their staff learns to use EHR platforms to their full potential.
Benefits of Adopting EHR Systems
The benefits of an EHR system can only be realized when your staff make it part of their workflow and start to take advantage of all the capabilities it offers.
1. Error reduction
According to a study in the British Medical Journal by Marty Makary, M.D. M.P.H., it’s estimated that medical errors lead to approximately 250,000 fatalities annually. They’re the third leading cause of death in the United States, behind heart disease and cancer. This conclusion is built on analyses of mortality data collected over eight years.
These errors can be misdiagnoses, misprescriptions, inaccurate laboratory testing, inadequate responses, etc. As innocent as they might be, medical errors can lead to severe patient injury or death and can cause practitioners severe anxiety, shame, or guilt. And, if a patient decides to go to trial, an average medical malpractice suit is settled for $242,000 out of court or $1 million.
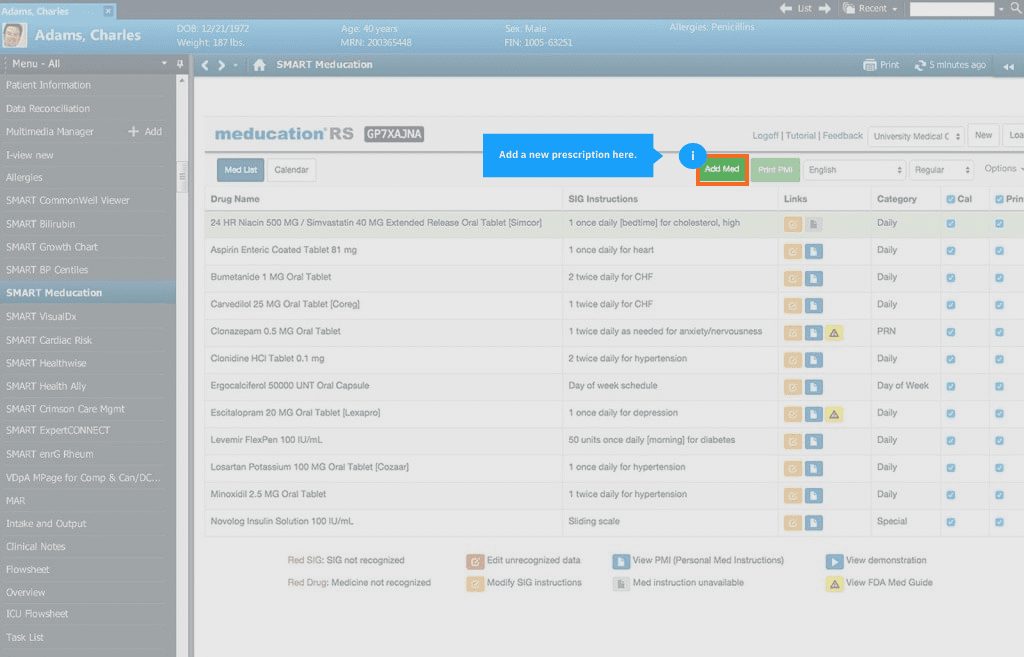
Electronic health systems eliminate many friction points where medical errors happen and reduce injuries and deaths due to misinterpretations, misdiagnoses, and human error. For example, American hospitals that switch to computerized physician order entry systems record a 66% drop in prescription errors resulting from doctors’ illegible handwriting and transcription errors.
EHR systems can be programmed to automatically notify nurses when they must dispense medication, alert them on administering the wrong drug (using barcode scanning technology), and store patients’ medical histories in one source that’s easy to access. This way, clinicians can focus on patient care vs. digging through cabinets and files from decades ago or trying to decipher medical cacography.
2. Safer and reliable workflows
Medical workflows help different departments communicate, collaborate, and focus on patient care without holding endless pre-round meetings every morning.
For instance, a workflow for ordering medication might include steps such as:
- A consultation session where a patient shares their symptoms.
- The doctor shares the results of the patient’s lab tests and explains the issue.
- The specialist prescribes medication for the patient to purchase at the hospital’s dispensary.
- The patient takes the prescription down to the pharmacy to get it filled.
If this workflow is run manually, several points of failure can be encountered:
- The specialist’s handwriting might be illegible
- The patient’s test results might mix up with another patient’s
- The prescription might get lost in the patient’s custody.
On the other hand, here’s what the workflow will look like when run on an electronic health system:
- During the consultation, the doctor pulls up the patient’s test results uploaded to the EHR by the lab department.
- The doctor shares the findings with the patient, prescribes medication, and registers their prescription in the EHR.
- When the patient gets to the dispensary, the pharmacist can access the doctor’s prescription from the EHR without straining to decipher some handwritten scribbling.
3. Improves patient experience, engagement, and management
There are several touchpoints along the medical workflow where patients start forming an opinion about your establishment, such as:
- Booking appointments
- Engaging with gatekeepers
- Wait times
- Consultation/treatment experience
An EHR helps clinicians offer patients a polished consulting and treatment experience that’s more likely to gain patients’ trust. Among others, EHR systems provide self-service patient portals that:
- Help practitioners give patients complete and accurate information about their medical evaluations.
- Offer continuity so that different specialists and departments can pick up where their colleagues left off without being confused with a patient’s medical history or appearing disorganized.
- Serve as a single source of truth where patients can keep track of their medical records, appointments, prescriptions, and doctor’s notes.
4. Access to complete and accurate information
Over 20,000 prescription drug products are approved for marketing by the United States Food and Drug Administration, plus at least 6,700 medical device product categories the agency oversees.
Given the scope of active substances doctors work with, it’s a given that they will inevitably mix it up at some point. According to Cross River Therapy, 1.5% of hospital prescriptions have dispensing mistakes, and one out of five Americans have been involved in a medication error when being provided health care.
Electronic healthcare systems can flag contraindications for specific prescriptions or combinations, food and drug interactions, duplicate therapy, drug-to-allergy reactions, and potentially conflicting instructions from different specialists.
5. Lower operational costs
An article by Tina Highfill, a Senior Research Economist at the United States Bureau of Economic Analysis, shows that hospitals that adopted EHRs with even basic capabilities had 12% lower average costs than their peers. And why not? EHR platforms reduce repetitive manual tasks, help doctors focus on the patient experience, reduce errors, and above all, increase hospitals’ operating margins.
It’s important to note that EHRs are a significant investment that can eat up much of a clinic’s cash reserves. Still, they eventually return a positive ROI, especially if the hospital switches from not using an EHR to a hospital-wide adoption.
Challenges Impacting EHR Adoption
Here are some of the challenges that impact EHR adoption.
1. Security and data compliance
An electronic health system serves as a second brain for a hospital’s staff to rely on. It helps clinicians store patients’ medical histories, coordinate medical workflows, and reduce paper trails.
But, with that centralized structure comes the risk of attacks by hackers and ransomware operators. According to Sophos’ State of Ransomware in Healthcare in 2022 report, the average remediation cost for a ransomware attack is around $1.85 million.
A ransomware attack can eat up your hospital’s cash reserves since ransoms range from just $197,000 (for smaller clinics) in direct costs to as high as several hundred million when you factor in lost revenue, etc.
Even if you manage to avoid bad actors, you’ll come under scrutiny by the authorities. Healthcare regulators take medical data protection seriously. HIPAA penalties for offenses such as lack of oversight and neglect of data management protocols can fetch an assessment ranging between $63,973 and $1.9 million per violation.
2. Investment costs
According to a research brief by Neil S. Fleming, Ph.D. et al., the average five-person clinic spends around $162,000 on an EHR implementation and an additional $85,000 in maintenance fees in the first year. The figure scales up exponentially as clinicians are added to your staff.
A report by the Medical Group Management Association Center for Research and the University of Minnesota School of Public Health shows that purchasing and deploying an electronic health system costs roughly $32,606 per FTE physician you have on staff.
Now, if we account for the fact that hospitals can have anywhere from 11 days to 521 days worth of cash at hand, it’s easy to see that this financial investment might eat up a hospital’s cash reserves or push them into issuing bonds.
3. Resistance to change
Internal resistance is the single biggest obstacle to successful EHR adoption. And it’s a problem that only arises after you’ve made the investment. Certain members of your staff may be unwilling to commit to EHR adoption because of different reasons:
- Anecdotes from fellow medical workers who have struggled to use an EHR in their organizations.
- Poor computer literacy.
- A lack of perceived value.
- Unwillingness to disrupt trusty workflows that may have lasted for years.
4. Lack of support
EHR systems are complex and often updated with enhanced functionality, new features, software patches, and bug fixes. Some of these updates may change how your system works, and, as a result, your staff might need continuous training programs and access to expert maintainers to ensure they get the required knowledge and can keep working without disruptions.
5. Technical limitations of the software
EHR systems tend to be interoperable, and data can’t be shared between healthcare organizations that use different EHR platforms. Secondly, EHRs are only as accurate as the data source they’re plugged into. If their backend is not updated frequently with industry best practices, your electronic health system can recommend substandard treatments and therapy for your patients.
6. Continuous training
A recent study by fellows at the Navy and Marine Corps Public Health Center and the Uniformed Services University of the Health Sciences shows that up to 94.6% of medical professionals surveyed think they could improve their ability to use their clinic’s EHR systems. Another survey of 154 primary care physicians shows that 46% of respondents did not feel their initial training was adequate, and 75% thought they’d benefit from additional training.
10 Tips for Successful EHR Adoption
You need to envision what you’re trying to achieve, from before the first conversation you have with a potential EHR vendor, to when your deployment is done and ready to be launched. Here are some tips to help you create a blueprint for your EHR adoption.
1. Establish the objective, cost, and benefits
To establish end goals, start asking questions like:
- Why are we investing in an EHR system?
- How will this new EHR improve patient experience?
- How will the EHR systems simplify clinicians’ workflows?
- How much do we expect to save by rolling out an EHR?
You need to define your strategic goals and focus your efforts on a larger objective so that you don’t end up embarking on digital transformation, leading to some quite spectacular failures.
Secondly, you need to determine how much it’ll cost (i.e., a range of figures from different vendors) both for the installation and the total cost of ownership over five-year and ten-year terms, for instance. When you factor in recurring variables like hosting, servers, maintenance, and training, your initial estimates can balloon—it’s no wonder why EHR projects routinely exceed their initial estimate by 25%.
2. Build a roadmap
A technology adoption roadmap serves as a blueprint for how an organization plans to make a new tool part of its workflow. It helps you connect EHR implementation with your organization’s needs, keeps your adoption on track, and enables you to avoid overspending on your EHR deployment.
3. Internal and external communication to encourage participation
For successful EHR adoption, it is crucial to engage your staff throughout the implementation process and help them understand how your new EHR system will:
- Simplify their workflow
- Automate repetitive manual tasks
- Reduce their paper trail
- Help them share medical records across departments
You can opt for demos, 1:1 conversations with product experts, or a coaching system where department heads learn the ropes and help their juniors get immersed in using EHR for specific use cases.
4. Error-free and timely EHR deployment
Depending on the size of your organization and requirements, it takes anywhere from 60 to 90 days, to as much as eight months to a year for EHR deployement. It’s imperative to work with an experienced vendor that can provide a reliable timeframe within which your staff can prepare for the switch from their existing workflows to the EHR.
5. Run usability tests
For successful adoption, a system need to be user-friendly. Usability testing helps you confirm if your EHR’s user interface is suited to your staff’s day-to-day workflow. This requires taking it for controlled testing in real-life patient scenarios to verify whether the system’s UI is simple, natural, consistent, and legible enough to serve your hospital.
6. Implement continuous training program
Implementing continuous training programs is of utmost importance to boost the adoption of your EHR system across the staff. Employees must be trained on how to use the features and capabilities of the system effectively, in order to adopt it into their daily workflow. An effective training program includes a combination of 1:1 coaching sessions, webinars, online courses, and certifications designed to improve your staff’s proficiency with:
- Charting and coding
- Medical terminology
- Healthcare law and compliance
- Creating, scheduling, and managing medical records electronically.
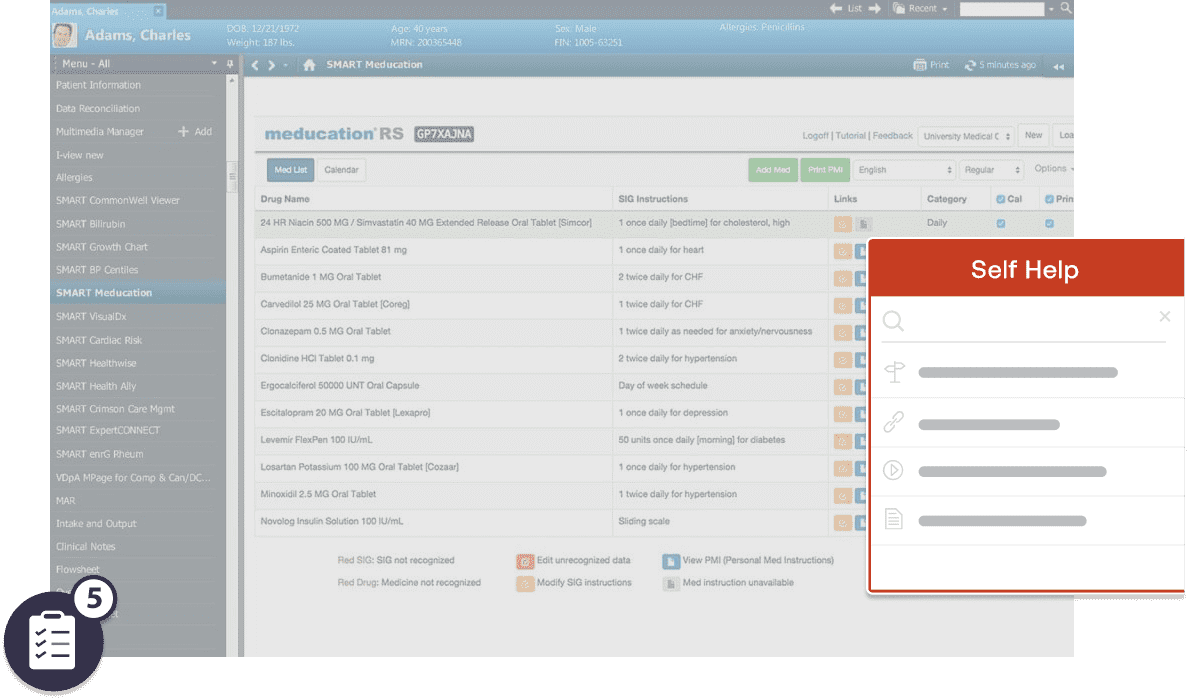
To implement effective in-app training programs, consider implementing a digital adoption platform such as Whatfix. Whatfix’s in-app guidance allows you to generate custom onboarding flows for any software in your toolkit. You can offer customized tooltips, popup recommendations, and a self-help widget that will pull the data from your knowledge base to support your employees all the way through the software adoption process.
7. Create EHR help and support content for your end-users
On-demand training and constant EHR end-user support makes it easy for your clinicians to get help with common issues without breaking their focus, interrupting their workflow, or waiting until a contract technician comes for routine maintenance.
Whatfix DAP can help your clinic create a library of product documentation, training articles, guides, explainer videos, and quizzes for your staff to access in the moment of need from any device, and inside the EHR interface.
Regina Owens, Director, Operations Learning and Development at AbleTo.
8. Monitor adoption and user engagement with product analytics and user behavior tools
Software adoption is an ongoing strategy. You need to monitor software usage to see how your employees implement software and what roadblocks they face. With these insights, you’ll be able to adjust your adoption strategy and offer more efficient training to your teams.
A product analytics suite, like Whatfix, can help track individual staff’s usage of specific tools, features, and resources, record their usage sessions, and detect where they may be facing issues.
9. Ask for feedback
You can hold 1:1 reviews, focus groups, or department-wide sessions where your hospital’s leadership tries to learn how your EHR has affected the staff’s workflow personally and on a departmental level and how you can assist their learning experience.
10. Evaluate and improve EHR onboarding, task documentation, and workflows
To improve EHR onboarding, you can use feedback to rework your adoption strategy. For example, you can:
- Enrich your learning library with bite-sized videos users can navigate on their PCs, mobile devices, etc.
- Schedule regular coaching sessions with third-party implementation partners.
- Set a longer timeline for your adoption efforts, especially if your staff feel they’re under much pressure to adopt the new EHR’s capabilities.
Whatfix digital adoption platform helps you get higher ROI on your enterprise software through context-sensitive onboarding and personalized training.
Whatfix offers product and guidance analytics to initiate the perfect handshake between users and your new software. It also helps identify key user behaviors within apps and track how people progress through in-app training.
Regardless of where your users are, Whatfix uniquely provides relevant, always available help, adapted from all sources across your company.
To learn more about how Whatfix drivers user adoption, schedule a personalized demo with us today!
Thank you for subscribing!