Electronic health records are at the heart of modern healthcare in the developed world. Since they went mainstream in the 1980s, they’ve seen massive adoption in countries like Australia (92%), New Zealand (97%), the United Kingdom (97%), and the Netherlands (98%).
The 2011 NAMCS Physician Workflow Study shows that most physicians agree that EHR adoption correlates with better patient care (78%), helps them access their patient’s medical charts remotely (81%), and alerts them to potential misprescriptions (65%).
If you’re at the stage where your organization is ready to invest in an EHR system, it’s understandable that you have lots of questions:
- How do we undertake the project? Does our EHR provider have the expertise required, or do we need to assist them with internal oversight?
- How much can we expect it to cost?
- How long will an EHR deployment take?
- How do we train our staff after setting up our EHR?
- What’s the best way to handle errors, bugs, and exceptions?
- Is it better to hire an in-house IT specialist or can we depend on contract partners?
- What responsibilities for compliance, data security, and reporting does an EHR system bring with it?
- What is the timeline for achieving high EHR adoption?
This article will help you understand how to navigate an EHR software implementation, no matter your healthcare provider’s size. We’ve supported each claim with peer-reviewed surveys and studies to ensure your implementation is successful, whether you’re a five-person clinic or a 500-bed hospital campus.
What Is EHR Implementation?
EHR implementation refers to the process required to set up electronic health record systems for healthcare organizations (such as hospitals, clinics, nursing homes, hospice centers, etc.), including:
- Enriching it with health data, patient records, etc.
- Building customer tasks, workflow sequences, and automation to reduce manual work.
- Communicating the change to medical staff and patients.
- Onboarding, training, and supporting your hospital’s medical staff on how the new EHR system works, how to use core features, how to troubleshoot errors, collaborate with teammates, etc.
- Cleaning and validating your existing data before record migration.
- Promoting na ew digital health records portal to patients, along with onboarding and support.
The Importance Of a Successful EHR Implementation
An electronic health record system is a significant investment, especially if you’re a smaller clinic. Every dollar needs to count to get a positive return on your investment and the time and energy your team spends learning how your EHR works.
Among others, a successful EHR implementation will help you:
- Reduce follow-on training, repair, and maintenance costs
- Speed up your staff’s workflow and reduce manual, repetitive tasks
- Better coordinate patient care across departments
- Create a single source of truth for all your patient data—diagnoses, prescriptions, medical histories, allergies, etc.
- Create a better, digital, modern patient experience.
How Long Does the EHR Implementation Process Take?
Depending on the size and requirements of your organization, you need anywhere from 60 to 90 days, to as much as eight months to a year to deploy an electronic health record system. This is also highly dependent on the size of your medical practices. For example, an EHR implementation for a small, independent clinic will be shorter and less complicated than a large, enterprise hospital network.
12 Steps to Successful EHR Implementation
The process of implementing an electronic health system is a puzzle with lots of pieces— feasibility planning, budgeting, deployment, training, and ongoing assistance to get a positive ROI.
1. Create an EHR implementation team
An implementation team must include stakeholders within your clinic, technicians on the EHR provider’s staff, and third-party support consultants to help you choose the right electronic health platform and design a procurement strategy to decide on the EHR provider.
Although EHR use cases usually differ, depending on the size of the organization, these core roles are a must for your implementation team:
- Project manager – to provide direction and keeps the project on schedule and within scope. The project manager also coordinates between the technical team and your clinic’s medical practitioners, whose feedback is used to customize the EHR.
- Application analyst – to collect requirements from a hospital’s departments and convert them into blueprints for the development team to code.
- Application developers – to build clinical applications for your staff.
- Quality assurance test engineers – to test run your EHR during and after the deployment to catch and fix bugs, errors, and exceptions.
- Super user and physician champions – departmental heads, senior specialists, and nurse leads who undergo training to learn how to use the EHR, integrate it with their existing systems, and educate their juniors and how the new systems work.
2. Define your budget, scope, and timeline
EHR systems cost hospitals roughly $32.6k per full-time practitioner and take anywhere from 60 to 120 days to deploy. The more questions you ask early into the exploratory process, the more you’ll get better, comprehensive answers that will help you allocate budget efficiently, avoid scope creep, and finish your implementation on schedule.
3. Communicate the EHR change early, as well as why it’s happening
Internal resistance is the only reason EHR implementation efforts stagnate or fail. To avoid pushback from your staff (especially if you’re a larger clinic), it’s essential to:
- Stage virtual and physical demonstrations that’ll show your nurses, GPs, etc., how an EHR will enhance their workflow, speed up their pace, and help them manage patient relationships easily
- Encourage staff to share their misgivings and address their concerns in detail
- Commit to a rigorous training program that will give your employees the confidence they need to use the new EHR system.
4. Understand all healthcare-related compliance requirements and security needs
Take time to learn the responsibilities you’re required to fulfill under statutes such as the Healthcare Information Portability and Accountability Act (HIPAA) and Health Information Technology for Economic and Clinical Health Act (HITECH).
5. Assess your hardware and infrastructure needs
After buying licenses for the EHR software to be deployed, you also need to account for:
- On-premise servers or cloud hosting on AWS, Azure, or Google Cloud.
- Scanners, monitors, medical-grade tablets, charging docks.
- Backup servers and uninterrupted power supply.
- Integrating with your other healthcare tech stack, such as your patient portal and healthcare CRM.
Although unusual, your EHR provider might offer software, hardware, and infrastructure as a bundle, in which case your budget will cover everything. But, if they’re purely a software vendor, you’ll need to budget separately for hardware, infrastructure, enhancements, maintenance, etc.
6. Map all existing EHR processes and create your new ones
With your new EHR systems in place, you’ll realize certain steps in your standard operating procedures have become redundant. At the same time, other processes are incompatible with the degree of functionality your EHR systems now offer.
First, you need to document your existing processes, highlight where they need to be adjusted or re-mapped, and then use those rough drafts to build better processes.
7. Clean and transfer your EHR data
Remove duplicate entries, fix structural errors, account for unwanted outliers, trace missing data points, and validate and run quality checks with your imported data points.
8. Provide role-based EHR onboarding and training
EHR user onboarding is the structured process of introducing healthcare professionals to a new Electronic Health Record system. This goes beyond basic software training and helps ensure all staff can use the system in their daily work. In fact, an excellent onboarding experience can increase early productivity by 70 percent.
Different users on your hospital’s staff will have different use cases for your electronic health records system:
- Registration clerks create patient profiles and enter their names, birth dates, gender, etc., into the system.
- Specialists, such as dieticians, radiologists, dentists, and ophthalmologists, use EHRs to store patients’ medical histories, diagnoses, medications, treatment plans, immunization dates, allergies, x-rays, and test results.
- Nurses study patient data and history stored on EHR systems to assist with symptom and function management.
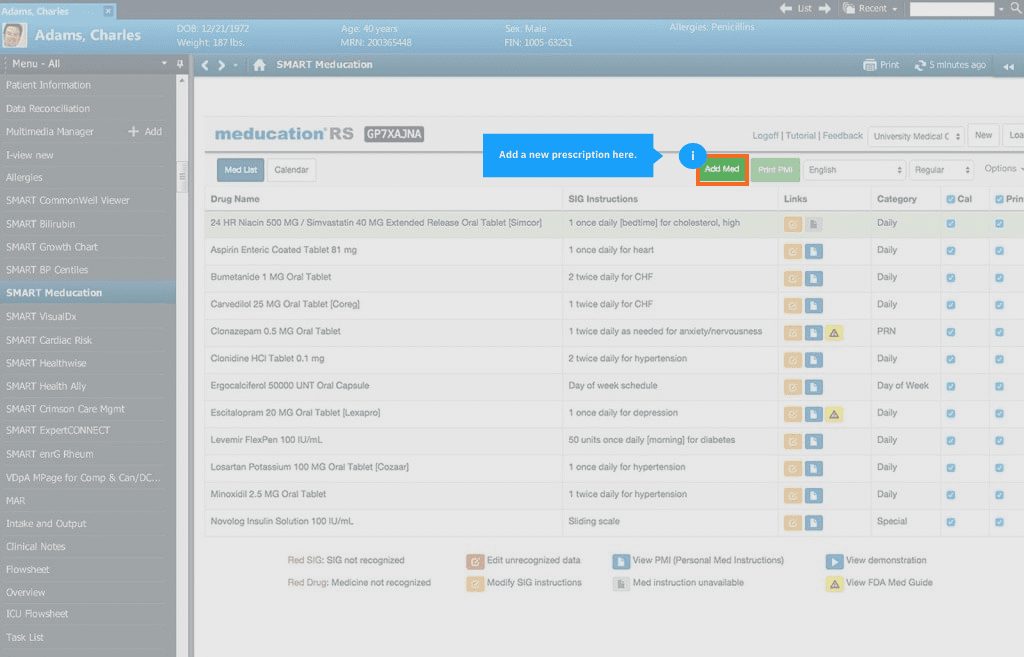
Healthcare IT teams can use Whatfix to enable EHR end-users with in-app guided onboarding and hands-on training.
With Whatfix Mirror, easily create replicate EHR environments that allow new EHR users to complete simulated tasks and engage with the platform for hands-on learning, all without risking live EHR usage or entering incorrect patient or medical data.

With Whatfix DAP, create in-app EHR user onboarding elements such as Tours and Task Lists to provide new users with a guided experience that lets them quickly realize value and understand how it is used to achieve their day-to-day activities.
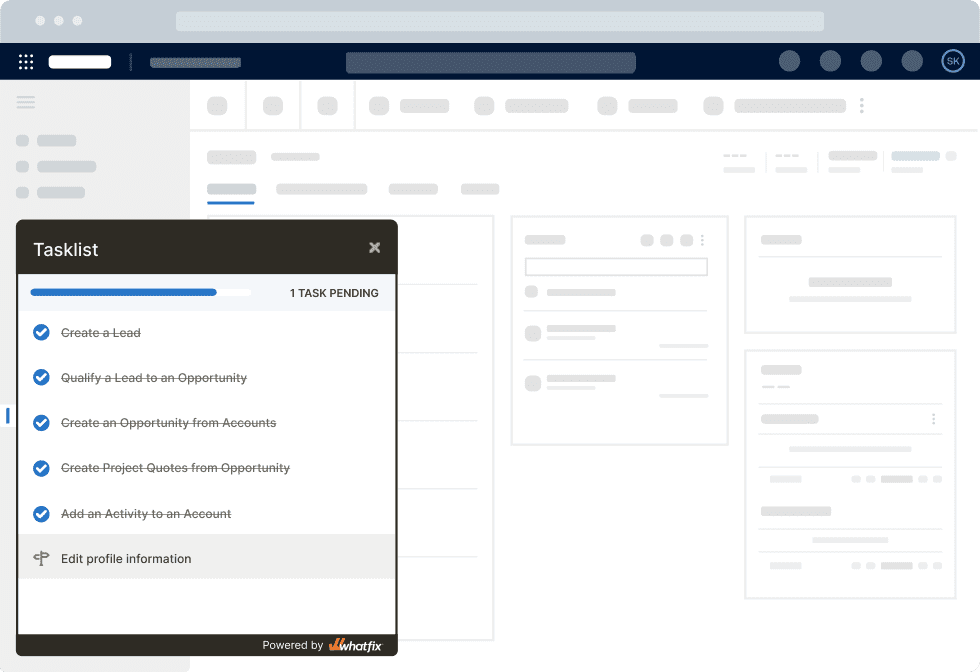
Your EHR end-users will require more than a one-time onboarding training experience to maximize your EHR investments ROI and drive healthcare outcomes. With Whatfix DAP, enable your healthcare works with Smart Tips that provide helpful context at critical workflow junctures, nudge them to take specific action, or provide additional knowledge. Use Flows to guide end-users through complex workflows or infrequently done tasks to support them in the flow of work.
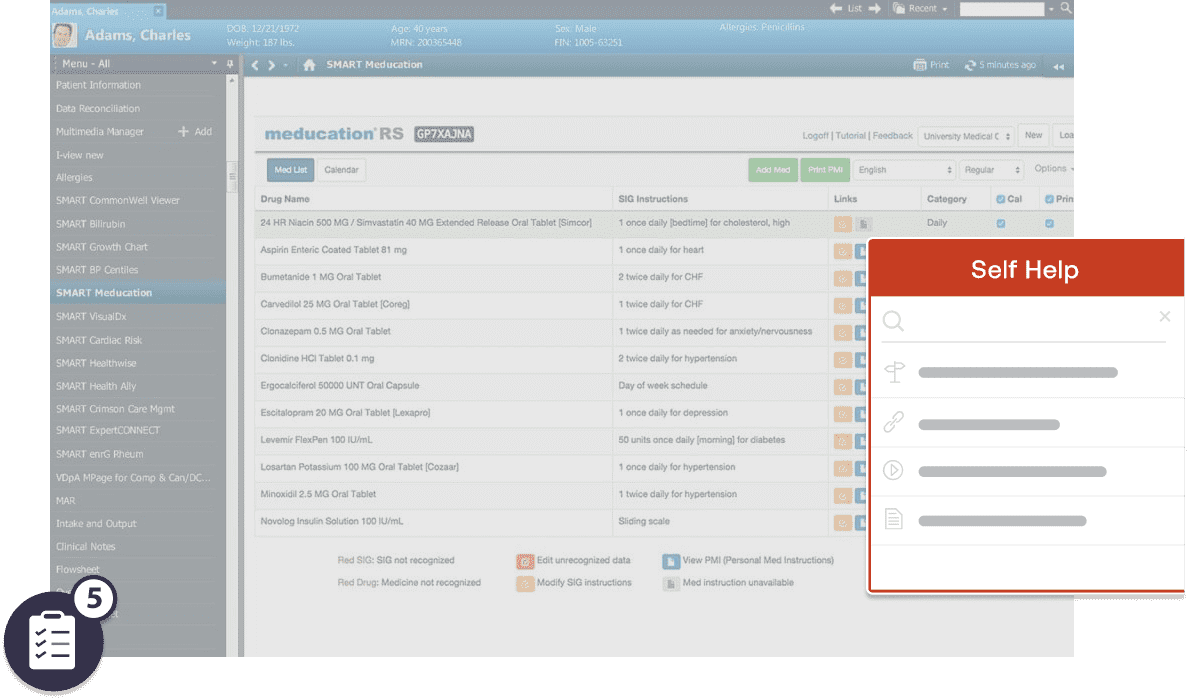
Whatfix DAP also supports EHR on-demand, anytime with Self Help, which overlays your EHR UI and provides a searchable help center that integrates with your LMS, EHR SOPs, training resources, videos, third-party links, and more.
This aggregates all your EHR processes and support documentation into one in-app help center. Whatfix tracks user searches to identify where support is needed more, helping you create new support articles or training sessions your users need.
9. Ask for feedback
A survey of 500 PCPs by Harris Poll, on behalf of Stanford Medicine, showed that although 63% of primary care physicians think their EHR systems led to improved care, only 18% of those surveyed are satisfied. 71% think EHR systems contribute to physician burnout, nearly half (49%) think it detracts from clinical effectiveness, and four out of ten believe an EHR system offers more challenges than benefits.
If you don’t want to pour hundreds of thousands of dollars into an EHR your staff won’t use, you must get their feedback during the QA testing stage. Start by asking questions such as:
- Has our EHR system improved your workflow?
- Did it give you more or less time to attend to patients?
- How much time do you spend engaging with patients vs. the EHR system?
- What do you think can be improved in our EHR’s interface?
- How much work do you need to enter and extract data from our systems?
The ultimate aim of electronic medical records is to automate tasks, streamline a doctor’s workflow and free them to engage with patients. If your EHR isn’t doing that in the sandbox stage, you might want to rethink your strategy.
10. Create EHR help and support content for your end-users
You need a library of self-serve resources your staff can access on-demand when they have questions or encounter bugs and errors. This can include product documentation, explainer videos, guides, and articles.
With a DAP like Whatfix, healthcare organizations can create an in-app self-help wiki that allows your staff and patients to search and find how-to and help documentation, videos, and links – all connected to related in-app guidance to showcase how to contextually complete a task or use a feature in the moment of need.
11. Take your EHR live
At this stage, your EHR has gone through the entire deployment process, QA has run its course, and it’s time to roll out your new electronic health records.
12. Monitor adoption and user engagement
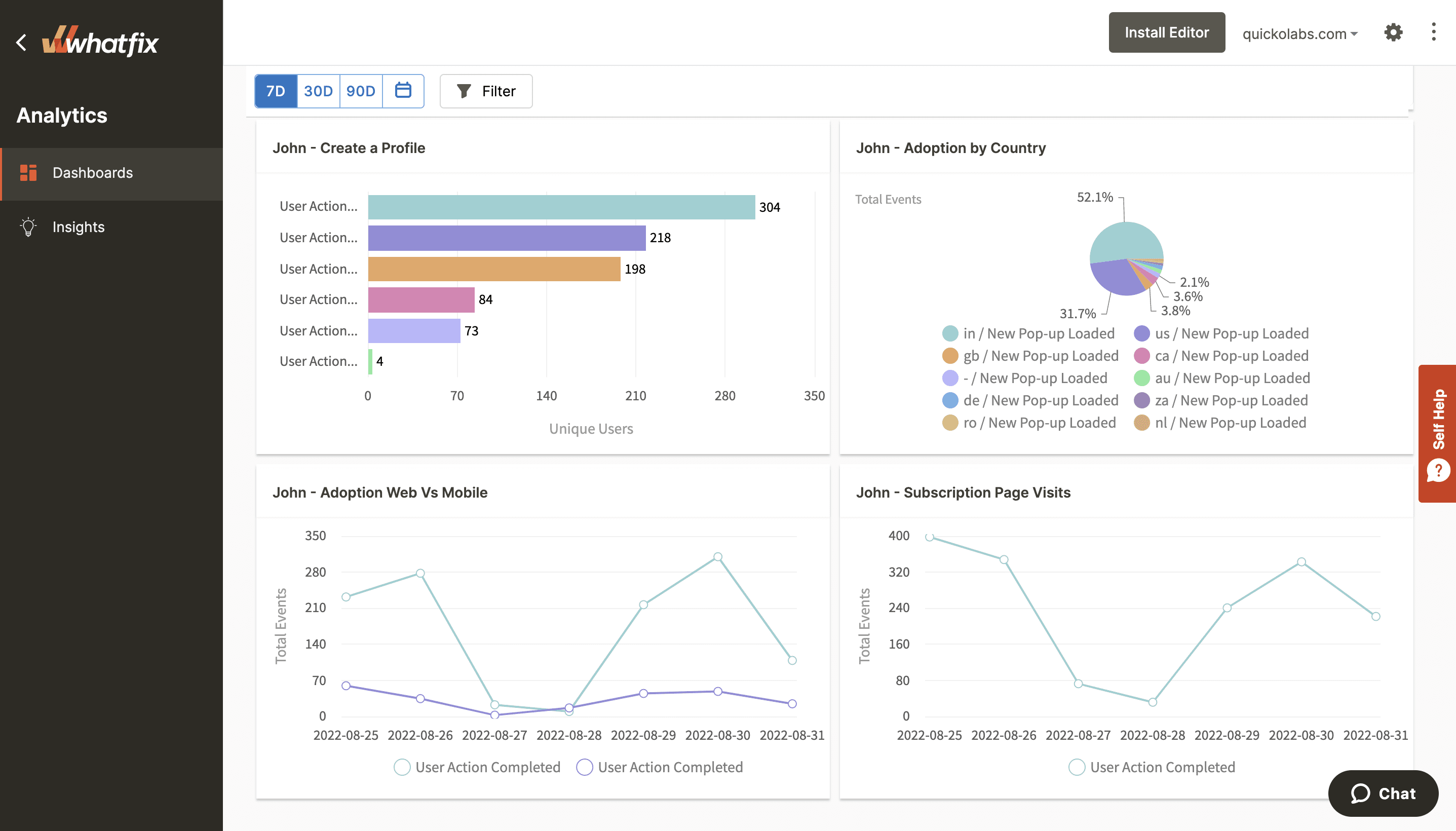
A product analytics platform like Whatfix helps you make the most of enterprise software with in-depth behavior analytics. Whatfix enables you to see who’s using your EHR platform, their use cases, the errors users run into, and how much they refer to help resources. This data gives you detailed insights into user engagement and the success of your EHR implementation.
5 EHR Implementation Challenges
EHR platforms are usually complex pieces of software that require a lot of financial investment, technical expertise, and ongoing maintenance to deploy. Here are five of the most significant challenges you might encounter as you roll out a new EHR product.
1. Cost
According to a research brief published in the Health Affairs Journal by Neil S. Fleming, Ph.D., Clinical Professor of Health Services Research, Baylor University, an average five-person clinic will spend around $162,000 on an EHR implementation, plus an extra $85,500 in maintenance fees in the first year.
Another 2005 study by the Medical Group Management Association Center for Research and the University of Minnesota School of Public Health corroborates that figure and found that an EHR purchase and deployment costs $32,606 per FTE physician. The study also discovered that implementing an EHR usually costs 25% more compared to a vendor’s initial estimates.
The bigger your clinic, the more you can expect to spend on an EHR deployment, and it’s not unusual for deployments to significantly exceed your budget. This can be problematic for smaller & mid-sized clinics, especially if an implementation starts to exceed their initial budget.
2. Employee resistance to change
Unsurprisingly, internal resistance to change and new information systems is the most significant challenge medical practices face with adopting electronic health systems, according to a paper by A. Kankanhalli, Ph.D. and H. Kim. A clinic’s staff (esp. nurses) might be apathetic or even resistant to the prospects of using electronic medical records, either because of:
- Unflattering feedback from their peers who have used and struggled with similar systems
- Poor technical expertise
- Lack of perceived value
- Unwillingness to disrupt their existing workflow
All these challenges lead to the reluctance to put in the work required to master an EHR, adopt it for the workflow, and use it consistently.
3. Training healthcare staff and patients
A study by fellows at the Navy and Marine Corps Public Health Center and the Uniformed Services University of the Health Sciences has shown that up to 94.6% of medical professionals surveyed think their ability to use their clinic’s EHR systems could be improved. In contrast, another survey shows that 75% of practitioners need additional training around five years after implementation to refresh their skills.
There’s no authoritative figure for the percentage of computer-literate medical practitioners. Still, if we consider that EHRs only started going mainstream around the 1980s, we can safely estimate that a significant number of GPs can’t use them confidently without ongoing training.
4. Data privacy and healthcare compliance
The United States Health Insurance Portability and Accountability Act of 1996 (HIPAA) is a federal law that requires the creation of health data standards to protect sensitive patient health information from being disclosed without their consent or knowledge.
The Office of Civil Rights enforces that mandate, and entities or individuals that knowingly obtain and share individually identifiable health details can be fined or imprisoned for up to a year. As of 2018, the average HIPAA fine was $1.5 million, and offenses such as lack of oversight and neglect can fetch an assessment ranging between $63,973 and $1.9 million per violation.
Electronic health systems serve as a second brain for medical practices and their partner. There’s always the tension between collecting enough data to build a patient’s profile, securing it, and storing it compliantly to avoid regulatory penalties.
5. Lack of communication
Nurses and GPs are more likely to be apathetic if you don’t communicate how an EHR will fit into their existing workflow. They’ll see it as a high-tech distraction designed to earn board members a promotion without regard to their entire organization’s workflow.
EHR Software Clicks With Whatfix
Accelerate your healthcare digital transformation efforts by enabling your employees and patients with contextual in-app guidance and constant real-time support via Whatfix digital adoption platform (DAP).
Whatfix provides EHR application owners and healthcare IT teams with a comprehensive no-code platform to enable EHR users, drive EHR adoption, and achieve healthcare business outcomes with frictionless digital healthcare experiences.
With Whatfix:
- Enable EHR end-users with contextual, role-based in-app onboarding and training with Whatfix in-app guidance with experiences like Tours, Flows, and Task Lists.
- Provide on-demand self-help support for EHR end-users with Whatfix Self Help and identify common troubleshooting issues with Guidance Analytics.
- Build EHR sandbox environments for simulated hands-on healthcare training with Whatfix Mirror.
- Collect EHR end-user feedback with Whatfix Surveys
- Analyze EHR end-user behavior to identify areas of digital friction and map optimal healthcare workflows with Whatfix Analytics.
With Whatfix, you can understand how your healthcare technology is used and under-adopted by your employees and patients. This makes it easier to adjust software onboarding, training, support, and overall end-user adoption strategies—all to provide a seamless experience for every end-user that enables them with the right context and support to utilize new technologies and systems fully.
Intrigued to learn more about Whatfix? Click here to schedule a free demo with us today!