Electronic Health Records are the foundation of healthcare’s digital evolution but installing the system is just the beginning. True transformation happens when your organization goes beyond technical deployment to secure clinician engagement and sustainable use.
EHR implementation remains challenging: just 38% of healthcare leaders say their implementations were successful, according to a recent 2025 Arch Collaborative report by KLAS Research. Without a disciplined approach to planning, training, change readiness, and adoption tracking, your EHR project risks stagnation or failure.
In this article, we’ll explore what meaningful implementation means, uncover common pitfalls, and share practical steps to ensure your project delivers on its potential backed by strategy and solutions built for healthcare transformations.
What Is True EHR Implementation?
EHR implementation isn’t a one-time event. True implementation goes far beyond installing software or surviving the first go-live week. It’s a strategic, multi-phase journey that ensures clinicians and staff not only use the EHR but use it effectively, confidently, and in a way that meaningfully improves patient care.
Implementation ≠ Adoption
Installing an EHR and flipping the switch on go-live doesn’t guarantee success. True EHR implementation requires both technical readiness and human-centered change management. That includes user training, ongoing support, communication, and clear metrics.
Examples of Partial vs. Full Adoption
| Usage | A physician who logs in to enter vitals | A nurse who uses the EHR to document vitals |
| Adoption | A physician who uses clinical decision support tools to improve patient care | A nurse who understands how to chart more efficiently using templates and automations |
The goal of true EHR implementation is to move all users from surface-level functionality to full, confident, value-driven usage across the care continuum.
Key Phases of EHR Implementation
- Planning and assessment: This phase includes vendor evaluation, workflow analysis, infrastructure review, stakeholder alignment, and resource planning. At this stage, healthcare leaders must align clinical, IT, and administrative goals with the EHR system’s capabilities.
- System configuration and customization: EHRs need to reflect how care is actually delivered in each organization. Customization should support existing clinical workflows and not force workarounds. Mapping templates, alerts, and data fields to user needs is critical.
- Go-live and initial rollout: This is the moment the system moves from planning into daily use. It requires intense support, real-time troubleshooting, and embedded onboarding for staff. Many organizations mistakenly consider the job done here but this is only the start.
- Stabilization and support: In the weeks following go-live, organizations must shift from fire-fighting to supporting adoption. End-users need in-the-flow training and contextual support. Change fatigue, resistance, and productivity drops must be proactively managed.
- Long-term adoption and optimization: This is where true EHR value is unlocked. Organizations that continue investing in training, feedback loops, usage analytics, and workflow enhancements see sustained adoption and satisfaction. This phase ensures the EHR evolves with the organization’s needs and delivers ROI.
Core Barriers to EHR Implementation
Even with high EHR adoption rates, the implementation journey is fraught with pitfalls especially when it comes to ensuring systems are usable, sustainable, and embraced by end-users. Poorly executed implementations often lead to burnout, duplicative work, and costly inefficiencies that compound over time.
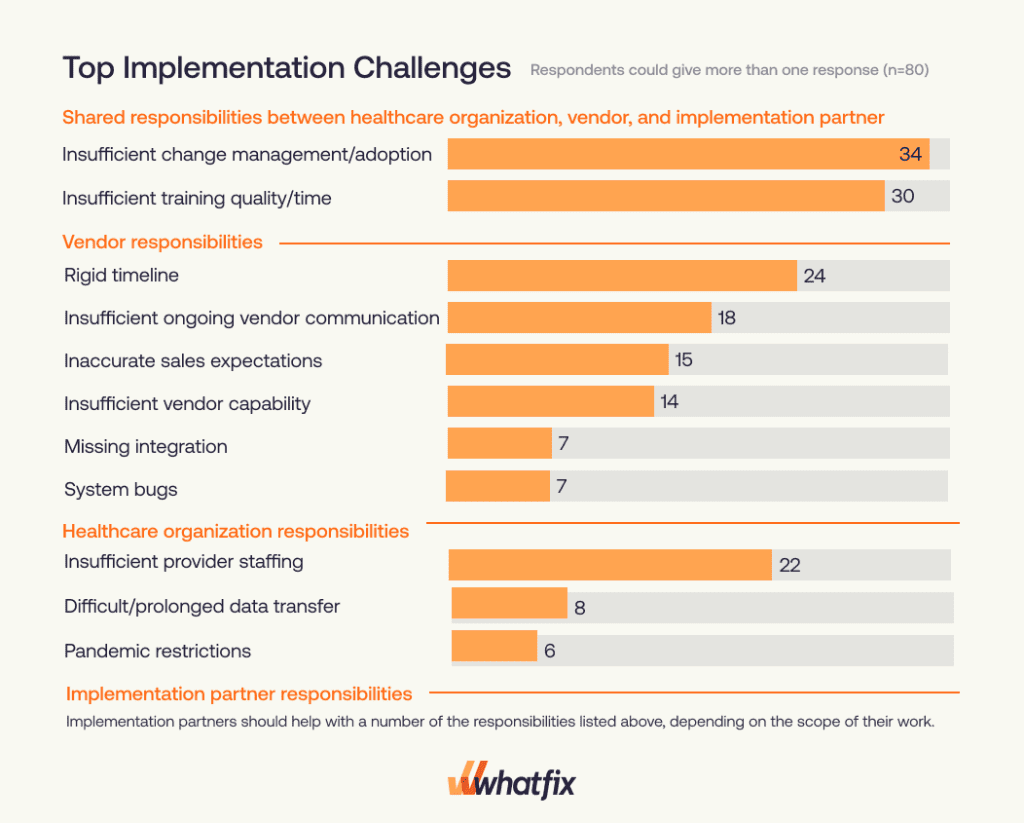
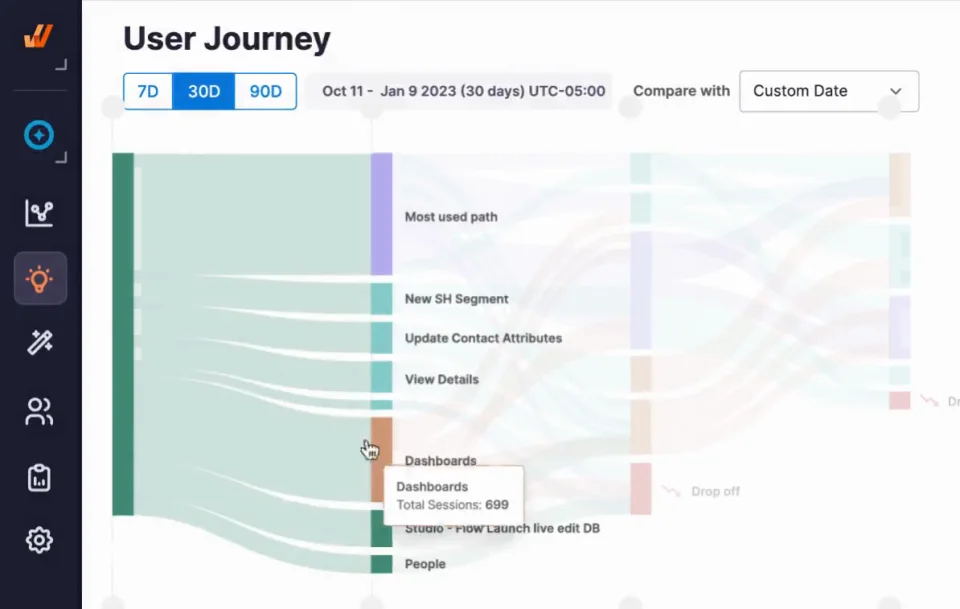
The chart below from the KLAS Arch Collaborative EHR Implementations 2025 Report highlights the top barriers as reported by healthcare organizations:
Let’s explore these and additional barriers that contribute to failed or suboptimal EHR rollouts:
- Insufficient change management and end-user adoption: According to KLAS, 34% of organizations cite change management and adoption issues as the top shared barrier between vendors, implementation partners, and healthcare organizations. Without leadership alignment, clinician buy-in, and end-user engagement, new systems are seen as burdens, not enablers. Becker’s Hospital Review also flags this as the most cited implementation failure point.
- Inadequate training time and quality: 30% of organizations report training as a key challenge. Most training is rushed, overly generic, or disconnected from real workflows. This leads to poor user confidence, increased errors, and long ramp-up periods that ultimately delay true adoption.
- Rigid timelines and poor vendor coordination: Vendors pushing rigid go-live timelines without adequate readiness create major risks. Additionally, 24% cite lack of ongoing vendor communication as a top issue. When vendors and implementation partners don’t collaborate effectively, organizations are left to bridge the gap.
- Technology usability and workflow fit: Even after implementation, usability friction, poor UX, and fragmented integrations between EHRs and other clinical systems create frustration. Clinicians struggle with clunky interfaces, redundant data entry, and inefficient navigation paths that increase cognitive load. Studies show this can increase documentation time by 11–22%, contributing to burnout.
- Resource constraints and staffing gaps: Nearly a quarter (22%) of healthcare organizations cite insufficient provider staffing as a top implementation challenge. Many hospitals, especially rural and mid-size systems, lack the bandwidth to dedicate full-time resources for configuration, training, and support.
- Poor data migration and system integration: Mismatched legacy data, prolonged transfers, and missing integration points add complexity. When data is siloed or inaccurate post-migration, clinician trust in the system drops and reliance on paper or shadow workflows increases.
- Limited visibility into implementation progress: Without behavioral analytics, teams can’t track where users are struggling, what features go unused, or how workflows are breaking down. This invisibility hinders early interventions, prolongs stabilization, and prevents long-term optimization.
A Strategic Framework for Successful Implementation (Powered By Whatfix DAP)
Successful EHR implementation is not just a one-time IT project, it’s an ongoing organizational transformation. From early stakeholder alignment to post-go-live optimization, healthcare leaders need a comprehensive, user-focused strategy. Here’s how to approach it and how Whatfix can supercharge every stage.
1. Align Stakeholder Goals Early
Engage clinical leaders, IT, and executive sponsors from the start. When all stakeholders are aligned on outcomes, whether improving care coordination, reducing admin burden, or ensuring compliance, the implementation gains strategic clarity. Early involvement builds buy-in and reduces resistance later.
How Whatfix Helps:
Whatfix enables early alignment through Product Analytics, which offers visibility into current software usage patterns, bottlenecks, and inefficiencies. These insights can be shared across stakeholders to unify priorities and validate assumptions. Product teams and IT leaders can use this data to prioritize workflow configurations and training modules that directly impact clinician productivity and care quality.
2. Validate Workflows Pre-Go-Live
Don’t assume your EHR design matches real-world clinical workflows. Conduct usability testing and shadowing to ensure the system supports how physicians, nurses, and admin staff actually work. Testing also uncovers interface issues, missing fields, and decision-support gaps that can lead to user frustration.
How Whatfix Helps:
Whatfix Mirror empowers IT and training teams to create production-like sandbox environment that replicate the EHR interface using anonymized or dummy data. This allows for rigorous pre-deployment testing of workflows across user personas. Mirror sessions capture behavioral data and qualitative feedback from test users, helping surface issues before they become post-launch blockers. With a safe environment to simulate clinical and operational tasks, you can refine workflows based on real user interaction and improve usability from day one.

3. Deliver Role-Based Training & Simulation
Generic training rarely delivers. Develop simulation-based programs that reflect real, role-specific scenarios like entering orders, updating medication lists, or billing workflows. Simulated training environments improve confidence, reduce anxiety, and minimize patient risk.
How Whatfix Helps:
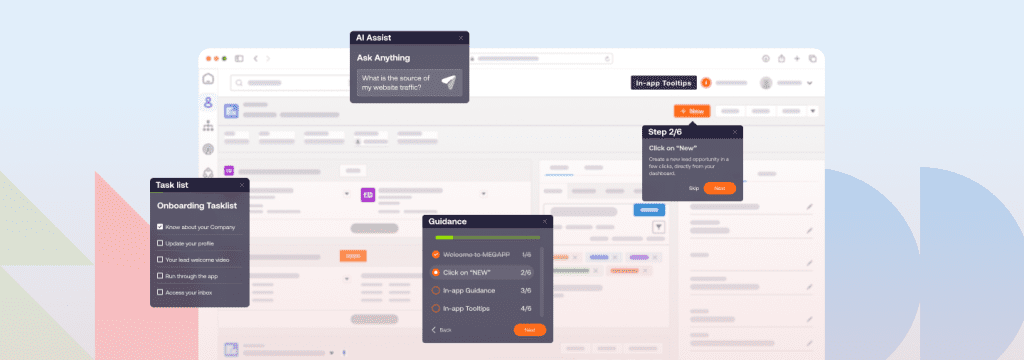
Whatfix Digital Adoption Platform (DAP) enables the creation of in-app, persona-based training experiences directly inside the EHR system. Using Flows, Task Lists, and Smart Tips, each user is guided through real-world tasks relevant to their role, whether that’s a physician updating care notes or a receptionist handling appointment workflows. These contextual, just-in-time learning interventions reduce onboarding friction, reinforce knowledge in the flow of work, and improve overall digital confidence without pulling users away for separate training sessions.
4. In-the-Moment Support & Change Communication
Post-go-live is where many implementations falter. Clinicians often forget training or struggle with new workflows under pressure. Provide real-time, contextual help embedded directly into the EHR and reinforce new policies or updates with targeted messaging.
How Whatfix Helps:
Whatfix embeds Self Help widgets, tooltips, and Smart Pop-ups directly into the EHR interface. For example, if a physician forgets how to update discharge notes, they can access a step-by-step walkthrough without leaving the platform. When process changes occur (like new consent form requirements), you can deploy in-app Beacons and Pop-ups to notify users and guide them through the updated process, no emails or LMS courses required.
5. Track Behavior, Not Just Launch
Measuring success purely by “go-live” misses the real goal: sustainable, meaningful use. You need to understand who’s using the system correctly, where drop-offs occur, and how training translates into performance.
How Whatfix Helps:
With Whatfix Product Analytics, healthcare organizations can track task completions, friction points, repeat errors, and training usage. You can build user segments (e.g., by department or role) and monitor adoption trends. This allows IT and L&D teams to identify who needs further support, refine interventions, and tie training efforts to business outcomes like reduced documentation time or fewer billing errors.
6. Reinforcement and Continuous Improvement
EHR adoption isn’t a one-time event. As systems evolve with new features, integrations, and compliance updates, your training and support must evolve too. Build continuous feedback loops to refine processes, close knowledge gaps, and keep users proficient over time.
How Whatfix Helps:
With Whatfix’s no-code content editor, training content, Flows, Smart Tips, and self-help modules can be updated and redeployed without engineering help. L&D and IT teams can collect in-app feedback, trigger surveys, and monitor adoption data to continuously refine support content. This keeps users up to date and confident, even as the system evolves.
EHR Software Clicks With Whatfix
EHR implementation is a high-stakes journey that doesn’t end at go-live. Driving real value requires ongoing support, behavior change, and workflow optimization. With Whatfix, healthcare IT leaders can empower every user, clinicians, staff, and patients, to navigate complex EHR systems confidently and efficiently.
Ready to accelerate your EHR success? Click here to schedule a free demo with us today!