As one of the most digitally mature sectors, insurance companies invest strongly in digital transformation, particularly artificial intelligence (AI). According to Zipdo, 67% of insurance executives believe AI will significantly impact the industry in the next three years, and over 80% of insurance companies are already planning to increase their investments in AI technology.
The modern insurance policyholder wants a hassle-free, self-service experience, is mobile-savvy, and is happy to buy policies from new players in the insurance industry – also known as InsurTech companies – if they can provide these experiences. In other words, consumers prefer insurance companies that have already made their digital transformation.
If your insurance business hasn’t already, it needs to begin digital transformation. In this guide, we’ll cover everything there is to know about digital transformation in the insurance industry.
What Is Digital Transformation in Insurance?
Digital transformation in insurance refers to the process of implementing cutting-edge technologies to improve every aspect of insurance companies. Examples include using online claims portals, automated fraud detection, claims management software, and more.
9 Examples of Digital Transformation in Insurance
Emerging technology and cloud software have disrupted the insurance sector, transforming internal operations, employee experience, policyholder experience, and core insurance workflows.
Here are nine examples of digital transformation in the insurance sector:
- Automated underwriting using algorithms to generate contextual policyholder quotes
- AI & automation reducing claims processing time & cost
- Omnichannel customer experience tools improving policyholder communication
- Telematics technology enables personalization at scale
- Digitalization of legacy insurance applications and processes
- Blockchain and smart contracts add transparency to P&C insurance industry
- Digital adoption platforms improving agent productivity & performance
- Predictive insurance analytics
- Policyholder portals
1. Automated underwriting using algorithms to generate contextual policyholder quotes
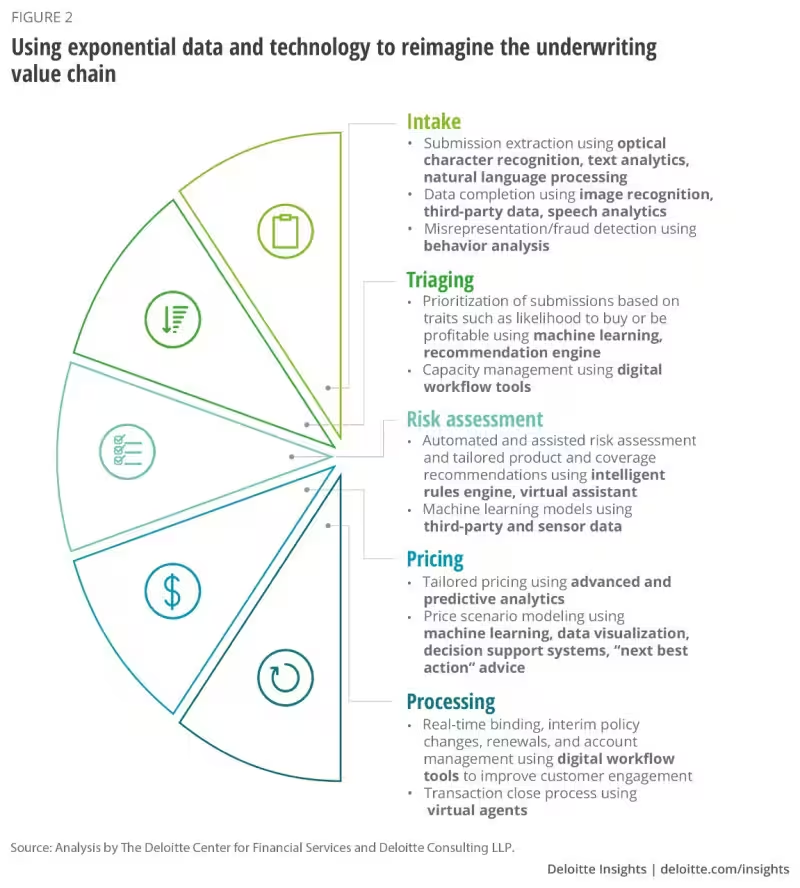
Automated underwriting is a computerized process where robotic process automation (RPA) software and artificial intelligence use algorithms to generate insurance quotes and underwrite the potential risk of clients, taking out the need for real people. This helps insurers with a more streamlined, less biased, and overall better underwriting process to assess, estimate, and price risk using aggregate or personalized data.
Once an algorithm completes its calculation, an industry professional reviews the quote or decision, investigates the logic behind why the automated underwriting system recommended the result it did, and adjusts if necessary.
Take Fannie Mae, for example. Its Desktop Underwriter system recommends decisions for mortgage lenders like “refer,” “refer with caution,” or “approve.” Mortgage lenders want to issue more loans but must do so cautiously to minimize financial risk. When a lender gets a “refer” or “refer with caution” recommendation from the automated system, they’ll either underwrite the loan manually or reject the application depending on specific risks identified by the algorithm.
P&C insurers use a similar process to assess risk and price policies, such as homeowners’, car’s, and renter’s insurance. Approved customers can digitally sign up for a policy without speaking to a human underwriter through self-service experiences. If appropriate, a P&C professional can manually amend a policy once the customer is insured.
With automated underwriting systems or loan software, those applying for insurance can complete the process without speaking to a real insurance agent. The number of consumers willing to do that has skyrocketed over the past few years – from 17% in 2016 to 36% in 2020, an increase of over 110%.
2. AI & automation reducing claims processing time & cost
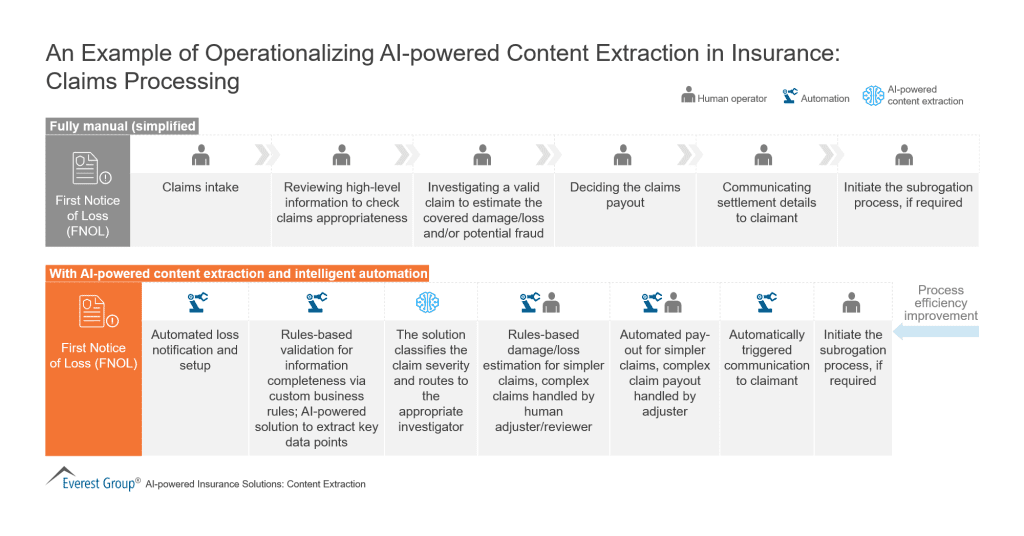
Manual claims processing typically takes around 30 days or more. And because many people are involved in the process, it’s susceptible to human error. Artificial intelligence (AI) and machine learning tools, on the other hand, reduce claims processing error rates to 0% and speed up the process by one to 15 days. AI has also decreased processing costs by 30%.
AI and machine learning tools continue to improve their effectiveness at identifying potentially fraudulent claims and estimating damages and losses because they continually analyze relevant data. These tools can also be programmed to handle repetitive tasks, like filing the first notice of loss (FNOL), freeing up time for your agents to do more thought-intensive activities.
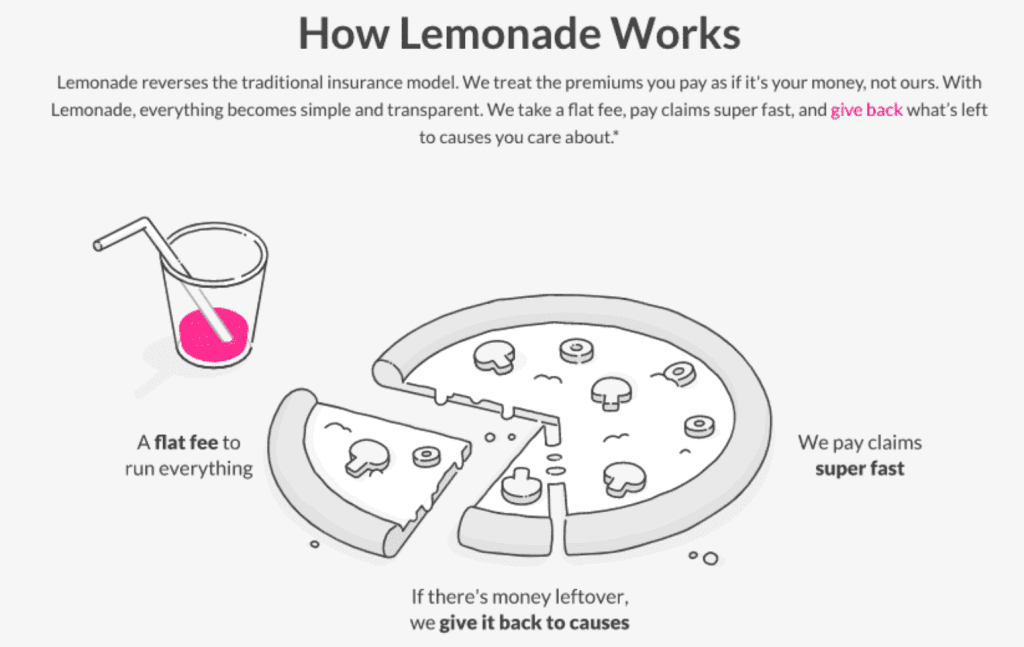
One AI and machine learning tool changing the insurance landscape is Lemonade, an InsurTech startup with an automated chatbot that has achieved the unimaginable: it processed a digital insurance claim in three seconds, from filing to payout. It has also identified a large number of insurance fraud attempts, saving insurance providers millions.
3. Omnichannel customer experience tools improving policyholder communication
Providing an omnichannel customer experience (CX) means meeting your customers where they are and communicating relevant information to them regularly. Your customers need to be able to buy policies, process claims, and more on both web and mobile devices. Insurance providers that meet those demands will find that their customers are more loyal and less likely to churn.
Omnichannel CX in insurance also means providing customers with easy access to information, accurate and predictive customer service, and fast processing times across all platforms. According to Salesforce, 58% of customers say their expectations have changed because of technological advancements, including omnichannel CX tools such as insurance chatbots. They want a more retail-like experience—easy access to your product offerings and quick responses from your customer service team.
Insurance chatbots help your firm educate customers, collect customer feedback, and run simple processes. Artificial Solutions’ AI-powered chatbot is a great example of a conversational chatbot that communicates with customers using natural language. Customers can ask the bot questions, buy policies, file claims, and more using a faster and more streamlined process. Customers have a great experience, and you save time and money in manpower and support.
4. Telematics technology enables personalization at scale
Telematics technology is data tracking software and hardware (think your cell phone, website cookies, global positioning systems [GPSs], and computers) that track users’ behavior with their consent. Before telematics, there was no way for insurers to track and influence policyholders’ behaviors. Insurers couldn’t assess risk on an individual level at scale, so they had to create policies based on general data instead of personal data.
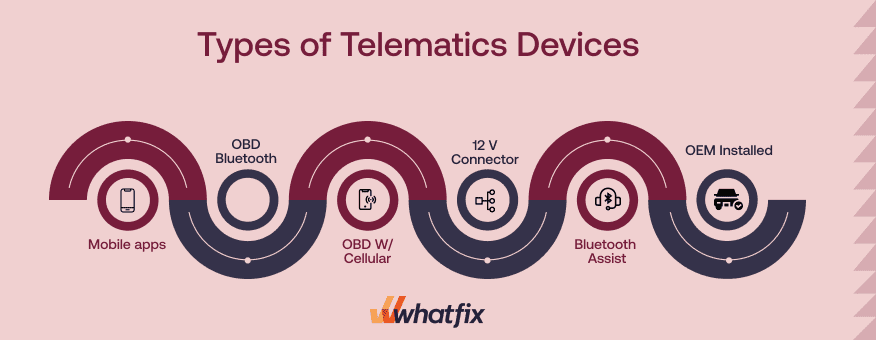
Auto insurers have already started using telematics tools like GPS trackers and beacons to track data directly from customers’ cars and devices. With that data, insurers can anticipate changes in individual behavior to measure and reduce risks.
Insurers who use telematics and get the consent of their policyholders to track individual data can personalize policies and offer discounts that would not be possible otherwise. For example, instead of basing driving behavior on the general population, insurers can track an individual’s average driving speed, most-used route, rate of car usage, and more to give their customers policies that perfectly suit their needs.
Besides tracking behavior, telematics has also enabled providers to influence behavior to reduce accidents. Fewer accidents mean fewer payouts. Insights from telematics help insurers make better decisions around underwriting and claims, in addition to personalized policies.
Insurers have also started looking at smart home devices outside of the auto insurance industry to further drive P&C insurance digital transformation. Smart home devices track home data, such as humidity and temperature, that can cause damage to a home over time.
5. Digitalization of legacy insurance applications and processes
While legacy systems may have supported your insurance company in the past, these outdated applications and manual processes will eventually start to hold your company back. As legacy systems become outdated, they slow teams down, are difficult to maintain, cause frequent outages, and make it difficult to achieve your digital insurance strategy.
Legacy application modernization refers to insurance companies replacing outdated systems with modern, cloud applications. This may involve adding new SaaS solutions, migrating to new ways of doing things, and retiring legacy apps.
Common examples of enterprise insurance companies modernizing their legacy applications include:
- Implementing a new claims management system to automate claims.
- Launching new policyholder portals to provide self-service experiences for customers.
- Modernizing internal operations, like implementing a new HCM system.
6. Blockchain and smart contracts add transparency to the insurance industry
Blockchain is a digital ledger that records data in the form of “blocks” that become a permanent record once they are accepted “on-chain.” Blockchains are easily accessible by permitted parties through blockchain-based platforms. Smart contracts are lines of code stored on the blockchain that automate insurance claims processing to improve user experience and back-end efficiency. The smart contract is ultimately what would approve (or not approve) the conditions of a claim and send it off to be included in a block.
Without blockchain, when a customer decides to purchase a policy, there are four parties involved: the customer, the broker, the insurer, and the bank. But conversations only happen between two parties at a time—for example, the customer only talks to the broker, the broker only talks to the insurer, and so on. Information is passed from one party to another and gets held up or lost during the tedious back-and-forth.
It’s a long, convoluted process that lacks transparency and efficiency and usually provides a poor customer experience. It takes time for information from the bank to get back to the customer because that information has to go through two other parties.
Blockchain solves that problem because it is a decentralized system that removes the middleman and makes information more accessible. When a smart contract is created, it gets added to the blockchain for everyone to see. The blockchain-based smart contract then automates the tracking, management, and cloud storage of policies, records of physical assets, and claims-triggering events to increase back-end efficiency and front-end transparency. Instead of inefficient paperwork and slow communication, blockchain enables all information to be accessed by any party at any given moment.
To illustrate the process, the smart contract auto-initiates claims processing when certain conditions are met (e.g., policy expiration). Each piece of new information that gets executed through a smart contract gets entered into another block on-chain that would be accessible for all relevant parties to access.
7. Digital adoption platforms improving agent productivity & performance
Insurance digital transformation requires an upgraded tech stack and updated processes that theoretically save you time and money. But if your agents don’t know how to use your tech stack or complete your processes, then the time and money you would have saved are wasted.
Unfortunately, you can’t use traditional classroom training methods to train your newly digital workforce because they are outdated, time-consuming, and not collaborative enough for digital learning. You need to digitize and update your agent training methods to increase agent efficiency and reduce redundancy.
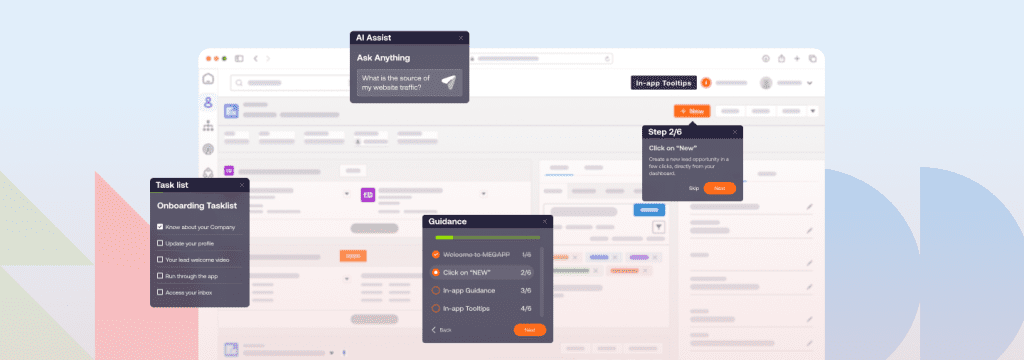
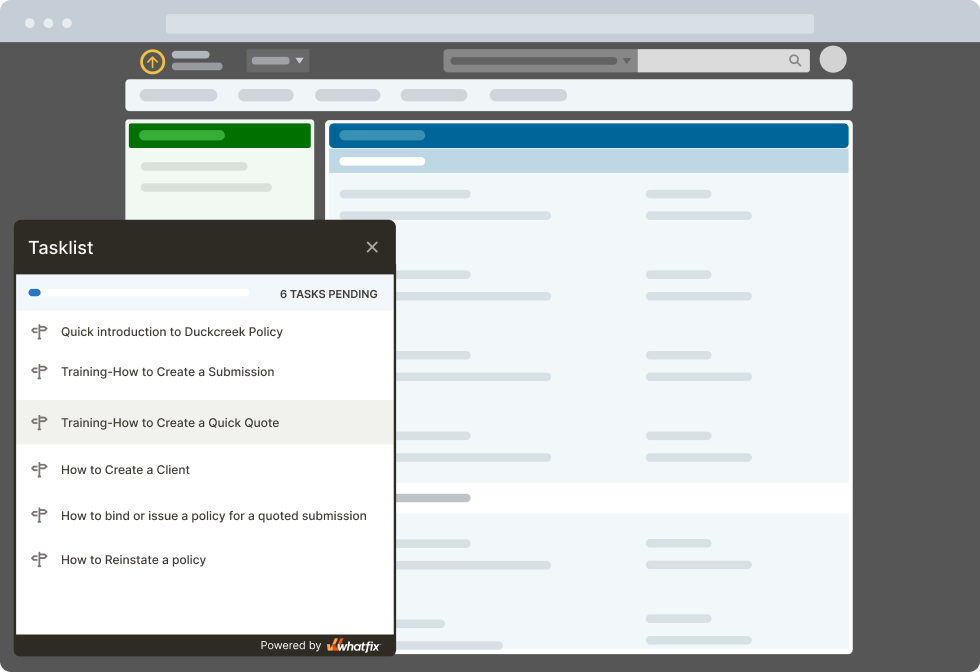
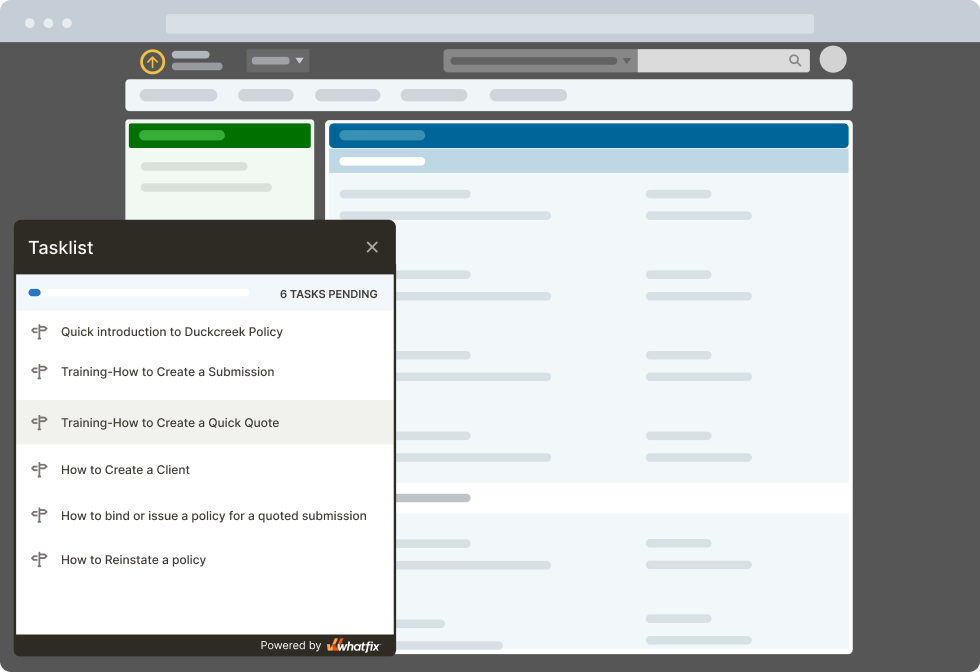
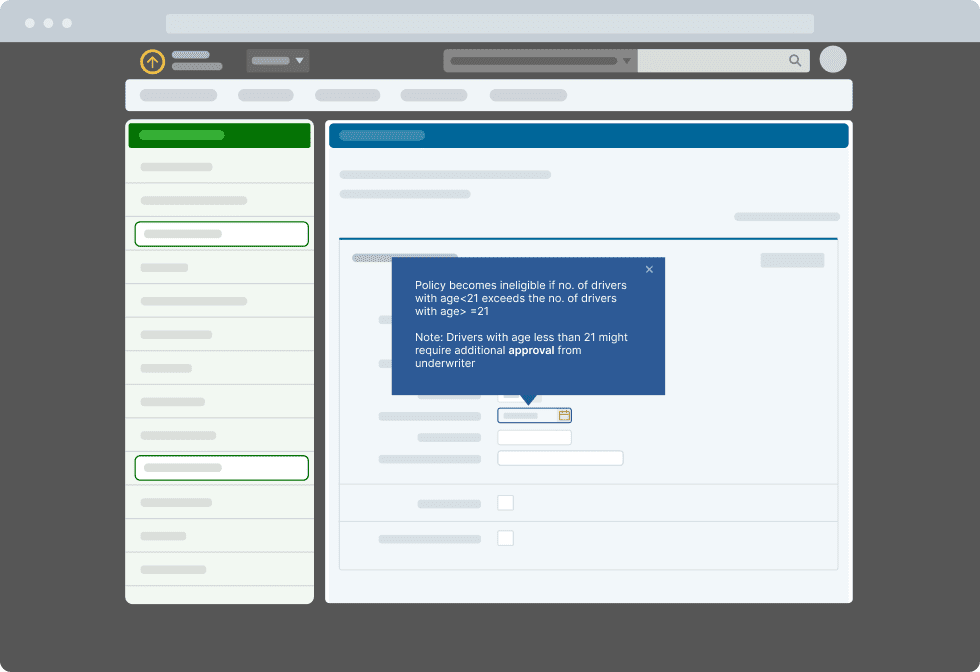
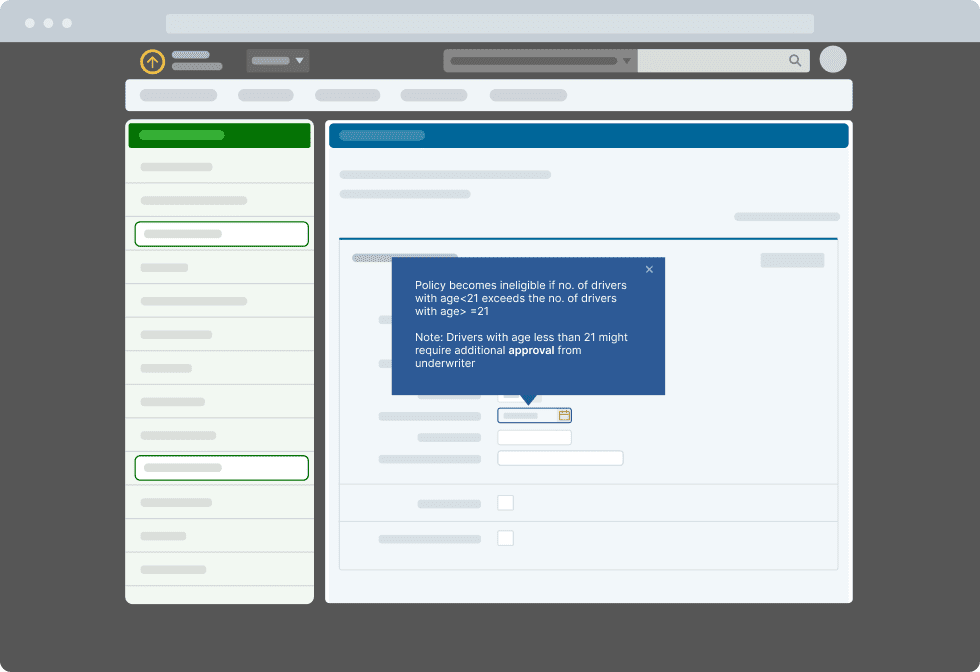
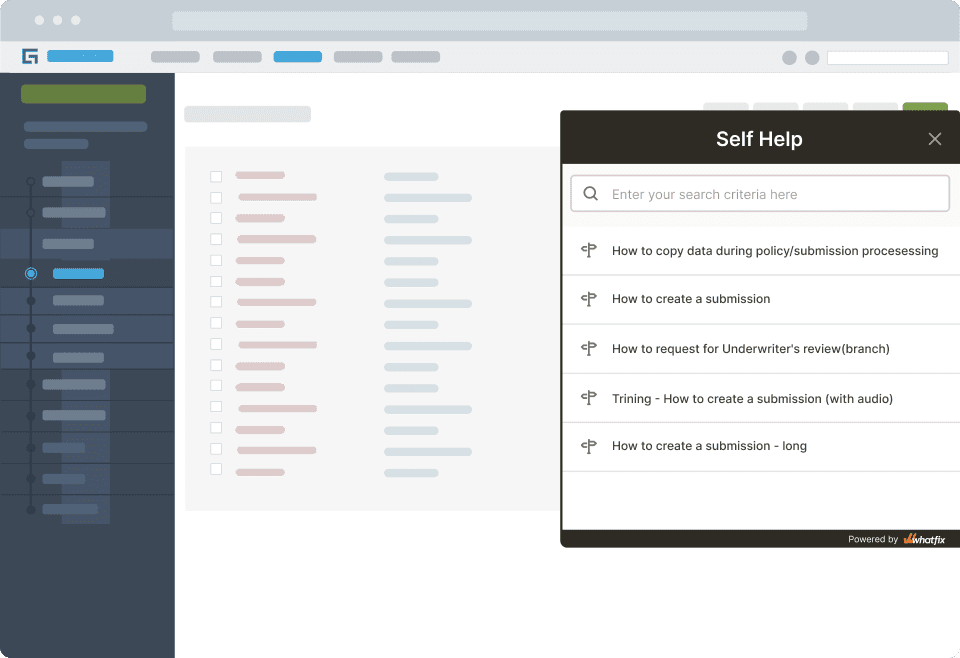
A digital adoption platform (DAP) like Whatfix DAP provides an “in-app” training technology that integrates with your applications and walks your customers and employees through important processes and new technologies, as well as provides an easily searchable Self Help content database.
With in-app guidance features like guided Flows, in-app Task Lists, contextual Self Help, guided Tours, Smart Tips, and Pop-Ups, employee and customer end-users are enabled to realize value and adopt new processes quickly. It also supports your employees by providing contextual, automated guidance technology to reduce errors and increase performance. Use all of DAP’s features to increase agent efficiency and improve the customer experience.
One example of how DAPs can drive efficiencies in the insurance industry is Sentry Insurance, which created end-user training 40% faster with Whatfix. They used Whatfix features to develop and deploy training modules across six different applications for over 77,000 people.
8. Predictive analytics
Predictive insurance analytics has always been a major aspect of insurance agents’ work. However, without quality technology at hand, they couldn’t gain accurate insights into customer behavior trends.
In the last few years, the data analytics landscape changed a lot. Now, agents can choose from a variety of tools and methods to perform accurate predictive analysis. They should stop relying on manual methods if they want to stay competitive and keep up to the standards set by InsurTech leaders.
Insurers have been reporting a positive effect of predictive analytics on reducing underwriting expenses (67%), sales growth (60%), and profitability (60%). The value of predictive analytics in insurance is only going to grow in 2024 and the upcoming years.
Predictive analytics tools allow insurers to collect data from different sources, identify patterns, and make more informed business decisions. To deliver predictive insights, analytics tools collect data from customer portals, customer relationship management (CRM), telematics, smart homes, and other systems that store information on insurance customer behavior.
Insurers implement predictive analytics to facilitate the following tasks:
- Insurance pricing and policy optimization
- Risk assessment
- Fraud detection
- Claims management
- Proactive customer engagement
For instance, by analyzing customer behavioral signals and buying patterns, predictive algorithms powered by machine learning can optimize insurance plans and offer more relevant insurance products to prospective or existing customers. Predictive analytics removes the guesswork from the policy pricing process, thus improving the customer experience and increasing insurance companies’ profits.
9. Policyholder portals
Over the last four years, the number of people who would switch insurance providers due to a lack of a user-friendly customer portal increased by 80%. Most insurance companies seem to take the statistics seriously – back in 2020, only 4% of European insurance companies didn’t have any plans for enhancing their digital capabilities.
With 74% of surveyed insurers enabling clients to manage their policies via mobile apps, custom insurance applications are now the most preferred channel for customer account servicing. But if you aren’t ready to invest in mobile app development, you can build a web portal as an alternative.
Benefits of Digital Transformation in the Insurance Sector
Insurance companies moving toward digital transformation feel positive ripples in their policyholder’s customer experience, their company’s bottom line, and their ability to scale and adapt to new processes.
- Improved customer experience for policyholders
- Reduced costs
- Increased scalability
- Reduced risks & frauds
1. Improved customer experience for policyholders
A digital transformation helps companies streamline the customer journey. Policyholders are able to access all information in one place: quotes for policies, claims prevention messages, first notice of loss, claims management, loss assessment, repair, and settlement. This aligns with customer expectations from insurance companies — timely wellness advice, a wide selection of policies, anxiety-reducing interactions, and quick payouts.
Digitally-savvy insurers can also offer customers:
- Lower premiums: Root Insurance aggregates policyholder data points such as driving habits, credit scores, demographics, and location to offer better deals to good drivers. One study found that about half of customers are happy to share behavioral data in exchange for such benefits.
- Faster claims processing: Insurtech Lemonade’s claims bot assesses and pays out claims in three seconds. It also provides quotes for renters and homeowners insurance in as little as two to three minutes and 24/7 support via self-service policyholder portals.
- More claims transparency: Standardizing claims calculations with artificial intelligence (AI) allows customers to see a complete breakdown of their claims. This also reduces the chances of litigation for insurers.
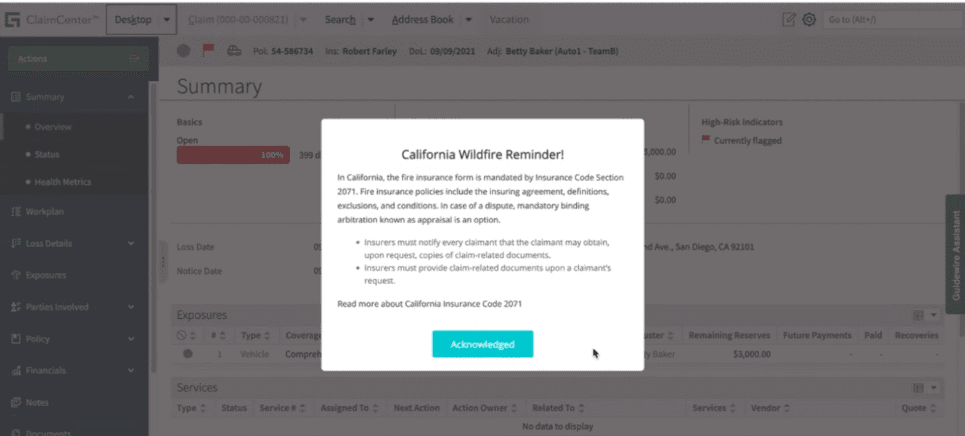
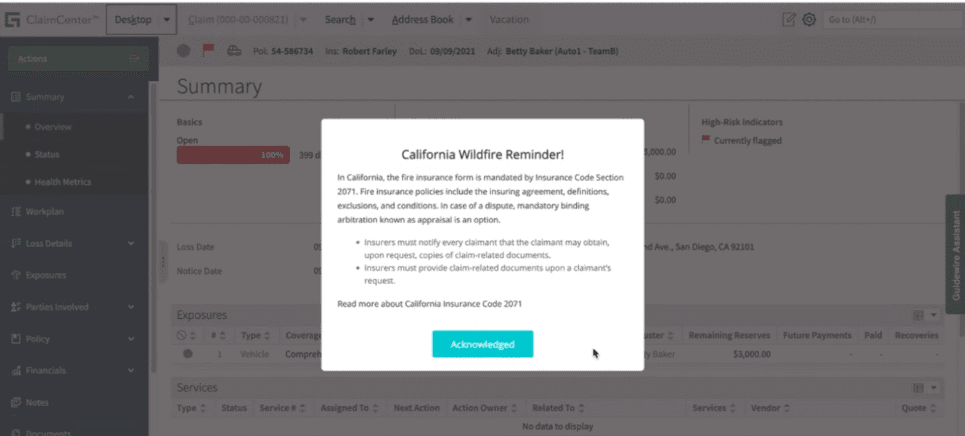
Whatfix + Guidewire Use Case: Overcoming Catastrophe Claims Processing Challenges With With In-App Guidance
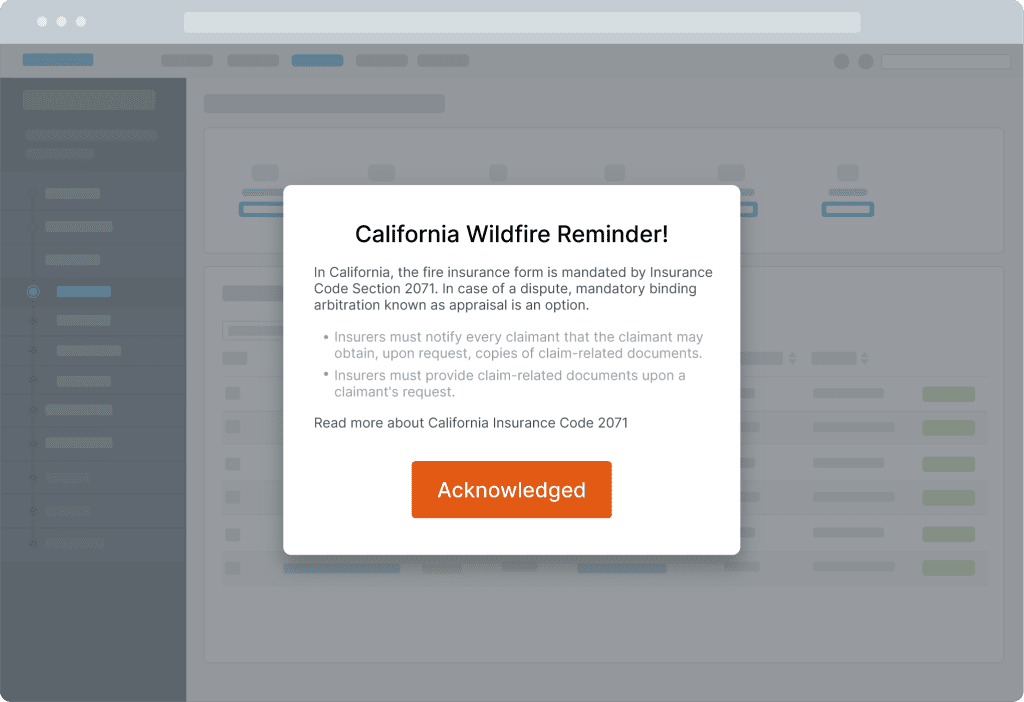
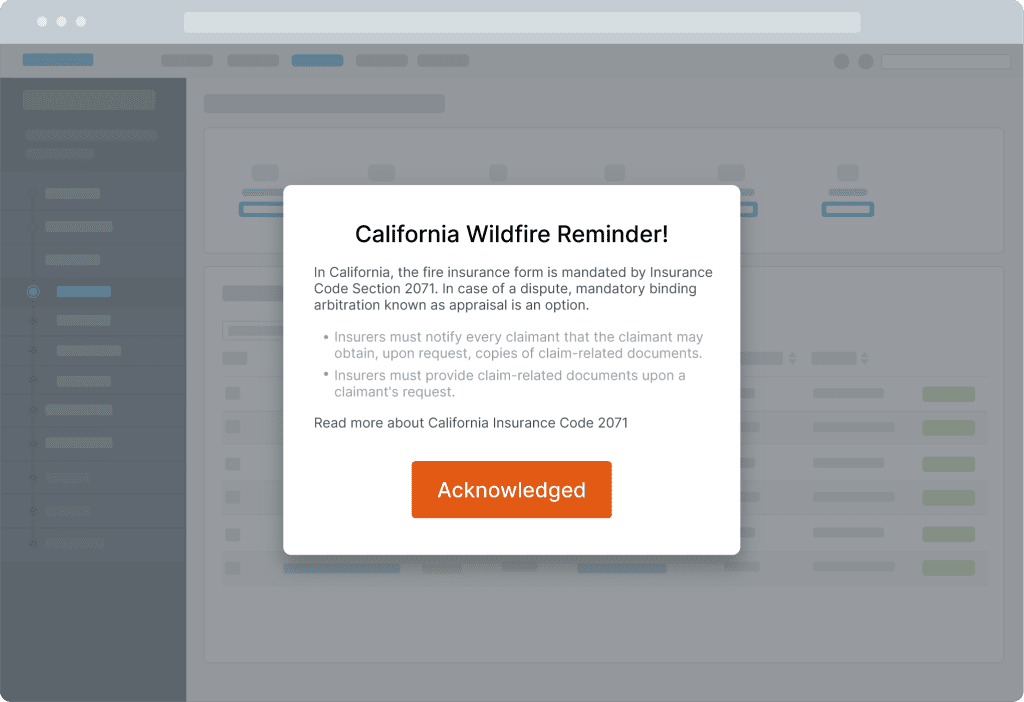
A Fortune 500 insurance provider enabled their claims agents with in-app Smart Tips overlaying their Guidewire claims process. This enabled claims agents with state-specific guidelines for rare events such as natural disasters in the flow of work, reducing claims times, enabling claims agents in the moment of need, eliminating data entry errors, and providing faster claims service to policyholders at times of disaster.
→ See how insurance technology clicks better with Whatfix
2. Reduced costs
Online self-service platforms, cloud storage, and automation improve efficiency and reduce the need for support and sales staff, which in turn reduces insurance companies’ operating costs. This focus on digital-first operations is why up-and-coming insurance tech companies already enjoy lower expense ratios (10-15%) than established insurers (25-35%).
A McKinsey survey done with US agents found that 44% of agents rated digital tools or customer tools as the number one capability insurers can invest in to support them. Employees want to use these tools to improve their workflows.
With suitable insurance applications and claims agent support systems in place, processes can be smoothed out internally. The ripple effects reach customers through faster response times, more accurate risk assessments, and lower premiums. It’s a win-win: Customers get what they need quickly, and insurance companies can better manage both productivity and costs.
Lower costs mean higher profits. As per one report, Ping An Life Insurance’s P&C unit grew operating profits 70.7% YoY, thanks to its investments in loss assessment and customer profiling technology.
3. Increased scalability
Self-service digital platforms allow companies to serve more customers while reducing pressure on customer support staff.
Case in point: AXA’s broker platform helps 3,000+ brokers see the status of the claims in real-time, identify suppliers, and track the next steps. Prior to using the platform, the company struggled with a never-ending stream of status update calls and low broker retention.
Another example of the benefits of P&C scalability is in catastrophe claims processing. When disasters, providers, and agents need to scramble quickly to provide great customer service and process claims quickly for policyholders that have gone through a traumatic event and make sure they’re comfortable.
4. Reduced risks & frauds
Smart devices in homes, cars, workspaces, wearables and drones help P&C insurance providers monitor policyholder activity and gauge risks. When a claim is filed, they help assess the damage and reduce instances of fraud.
The SmartRide program by Nationwide tracks miles driven, nighttime driving, hard braking, and acceleration to offer appropriate quotes.
Analytics and artificial intelligence platforms help insurers identify false claims. They refine social and publicly available data and apply it to claims decision-making.
Challenges for Insurance Digital Transformation
Seventy-three percent of enterprises failed to derive any benefits for their business from digital transformation. Here are some of the top insurance challenges when it comes to digital transformation:
- Inefficient change management
- Dependence on legacy systems
- Talent shortages and training challenges
- Regulatory compliance
- Claims processing and fraud
- Risk assessment and underwriting challenges
1. Inefficient change management
Digital transformation causes companies to “change the organization, talent model, policies, processes and procedures—basically, the entire service model or business model,” as Peter Bendor-Samuel, CEO of Everest Group, notes. Leaders who fail to manage this change will struggle with digital transformation.
It’s no wonder 42% of companies cite change management as an important factor in digital transformation. To reap the benefits of a digital overhaul, leaders must clearly communicate the degree of change and retire old processes. Merely implementing new technology is not enough.
2. Dependence on legacy systems
Like many sectors, the insurance industry has faced challenges adapting and adopting rapid technological advancements. This digital transformation has changed how insurance providers model their businesses, provide services to customers, and operate internally.
While the benefits of new technology and digital advancements present massive opportunities and growth for providers, the legacy application modernization process creates challenges such as guiding policyholders and employees through the transformation, developing new digital business processes and applications, retiring legacy applications, rethinking traditional business models, upskilling and supporting technology end-users, and more.
A few examples of new technology and enterprise software insurance providers must integrate into their infrastructure and workflows include:
- Claims Management Software
- Policyholder Portals
- Life Insurance Policy Administration Systems
- Underwriting Systems
3. Talent shortages and training challenges
The quality of an insurance company’s workforce impacts its capacity to grow, adapt to changing markets, and provide exemplary customer service.
Everest Group found a lack of internal skills and talent to be a major barrier in technology adoption among insurance companies. There’s also a high skills gap in three major areas driving innovation in insurance: artificial intelligence, cybersecurity, and the Internet of Things.
Insurance companies also need to train employees once they switch to new systems—inadequate training results in low adoption and little value for employees.
One survey found employees considered adequate tools and proper training important job characteristics. When employers failed to provide adequate training, employees found their jobs difficult and were more likely to leave. This is further strained by the fact that 400,000+ insurance employees are expected to retire in the next two years, and that 44% of millennials are not interested in a career in the insurance industry.
With a tool like Whatfix DAP and Whatfix Mirror, insurance organizations can drive user adoption of new applications like claims management tools or policyholder portals.
With Whatfix Mirror, L&D leaders can easily clone applications to create sandbox environments, enabling new agents to learn via interactive, hands-on training in a risk-free sandbox application.


With Whatfix DAP, end-users are supported in the flow of work with in-app guidance and onscreen overlays. Task Lists help new employees learn core processes, while Flows support employees on complex workflows or infrequently done tasks. Smart Tips provide additional context and nudge employees to take additional action. Pop-ups alert employees of process changes or company accounts, like regulatory changes. Self Help connects with your knowledge repositories and provides end-users with an in-app help center akin to a knowledge base.
4. Regulatory compliance
While undergoing a digital transformation, insurance companies must ensure that innovations comply with relevant regulatory mandates for data governance, security, and customer privacy. This requires a tailored approach, as various factors influence the specific regulations impacting operations.
For instance, integrating AI and machine learning can enhance risk assessment and customer service. However, these technologies must adhere to local data privacy laws. Insurance companies adopting such digital tools should invest in robust cybersecurity measures, employee training and upskilling, and regular third-party risk assessments to ensure compliance and security.
5. Claims processing and fraud
Processing claims and detecting fraud involves complex verification mechanisms that can pose challenges as fraudulent tactics evolve, when technology and resources are inadequate, and when processes aren’t standardized. The capacity to detect and prevent fraud is necessary to maintain the integrity of the company and the insurance industry. This is another area where digital transformation, advanced analytics, and even artificial intelligence are beneficial.
6. Risk assessment and underwriting challenges
Insurance policies and premiums are determined by risk and underwriting. These complex and dynamic factors require careful analysis and innovative solutions when issues arise. From cybersecurity threats, adopting new automated underwriting processes, data quality issues, ever-evolving regulations, and underwriter end-user errors, insurance organizations must remain agile to ensure the accuracy and quality of assessments.
How to Drive Insurance Technology Adoption
Digital transformation and adoption aren’t buzzwords in our current landscape. Insurance technology spending in the US and the UK is expected to grow by more than 25% between 2022 and 2026.
Digital capabilities help insurance companies meet the rapid pace of change across the sector. All to promote and sustain innovation from the back-end to the customer-facing front-end. According to Deloitte’s 2024 global insurance outlook, most insurers are realizing that reacting to risks may not be good enough and are undertaking transformation efforts aimed at preventing losses from happening in the first place.
Enterprises that take on digital adoption initiatives are better equipped to face challenges, capitalize on new opportunities, and meet the expectations of both customers and stakeholders in an increasingly digital world.
Here’s what insurance organizations can do to enable end-users, drive adoption, maximize transformation ROI, and achieve business outcomes:
1. Provide contextual onboarding and training
Insurance companies often have high turnover in their claims centers, contact centers, and policy underwriter departments. This requires insurance organizations to quickly ramp up new employees on how to use new systems and complete their tasks, all in a high-stress environment of upset customers dealing with accidents.
With Whatfix Mirror, organizations can create replica sandbox environments of their claims processes and insurance application tasks, providing hands-on training to new insurance agents without the risk of live software usage or processing real claims. This builds confidence in new claims agents, accelerating time-to-proficiency.


Digital adoption platforms (DAP) are revolutionizing insurance tech adoption by empowering end-users with contextual onboarding via in-app guidance and personalized learning paths tailored to each insurance agent’s role, tasks, and individual skill level. Consider a new insurance agent logging on and immediately receiving a customized interactive walkthrough of their tasks and a guided tour of the core platform features. This contextual approach ensures users learn by doing instead of passively consuming generic materials.
DAPs like Whatfix adjust real-time training based on end-user role, progress, and trouble areas, making skill-building efficient and engaging. For example, users can get the guidance they need if they encounter a common navigation issue. By providing the proper knowledge at the right time, DAPs empower employees and customers to work through learning curves efficiently.
2. Enable end-users with moment-of-need support
Users often need quick help overcoming roadblocks without losing momentum. DAPs like Whatfix deliver by providing in-workflow tips and self-help resource centers. For example, if an adjuster hesitates on a complex claims form, a personalized tip can instantly clarify the requirements to unblock progress. By integrating this assistance, DAPs promote user independence, satisfaction, consistency, and accuracy.
With Whatfix, create in-app support like Tours, Task Lists, Flows for interactive walkthroughs, and more that provide moment-of-need support for insurance professionals during their work and customers navigating new tools
With Whatfix Self Help integrates with your process documentation, training resources, video tutorials, help articles, SOPs, call center scripts, FAQs, knowledge base, and more – enabling employee and customer end-users with support at the moment of need.
3. Keep end-users updated on changes
As insurance technologies advance, keeping users updated on new features and process changes is essential, but challenging. DAPs meet this need through timely in-app notifications to share release notes, functionality upgrades, and more. All without disrupting workflows.
For example, a Pop-Up can alert claims managers about a new validation or process change and provide a quick start tutorial. Strategic DAP alerts keep the entire insurance workforce in sync with system changes.
4. Analyze end-user behavior for continuous improvement
DAPs like Whatfix add value by revealing how end-users interact with technology. End-user analytics can help you identify behavior patterns, pain points, and underutilized features. With this data, insurers can streamline digital platforms to better align with user preferences, manage adoption barriers through tailored training, and predict needs.
Continuous optimization driven by DAP insights also ensures that as consumer expectations evolve, the digital tools serving them do too. That way, enhancing user experiences and improving organizational agility feed into each other.
With Whatfix, track and analyze and end-user action with User Actions. This uncovers areas of end-user friction, maps user flows, builds user cohorts, and more. Use this data to create new in-app guidance and end-user support content, as well as continuously optimize and test new workflows and features.


5. Collect end-user feedback with in-app surveys
End-user perspectives offer invaluable direction for enhancing digital tools. DAPs like Whatfix support this feedback loop with in-app surveys and forms gathering user suggestions in their workflow. This convenience incentivizes participation, guiding refinements and new features.
Whether someone reports software bugs, requests for new capabilities, or feedback on onboarding experiences, this user input shapes a digital experience that aligns with real needs. Over time, direct user communication can lead to a community where customers and employees co-create better tech solutions based on end-user feedback.


6. Manage software subscriptions and licenses efficiently
According to Productiv, the average SaaS spend per employee in 2023 was projected to be almost $10K, while 53% of SaaS licenses go unused.
Managing several insurance software subscriptions can be challenging, but SaaS management platforms like Whatfix Enterprise Insights provide clarity into your software subscriptions and usage. By revealing end-user adoption rates for each solution, insurers can right-size investments to balance access with responsible spending, reduce SaaS waste, and optimize their digital strategy.
This helps cut overspending on unused tools without hindering employee productivity. With end-to-end visibility into usage trends and user sentiment, insurance finance and tech leaders can get more value by adding, upgrading, or retiring solutions as needed. The result is an increasingly optimized digital toolbox purpose-built for user needs.
Sentry Insurance Achieves Digital Transformation ROI With Whatfix
How might a DAP work for your insurance organization? Let’s look at Sentry Insurance, who partners with Whatfix’s DAP platform to support its digital transformation and end-user adoption initiatives.
Market shifts, changing customer expectations, and a new wave of insurance disruption required Sentry to act fast to support its digital strategy and enable its end-users. Associates need customer, policy, claim, and other data at their fingertips to deliver a great customer experience, respond quickly to claims, and find untapped growth opportunities.
Sentry used traditional methods and simple tools to point Sales, Customer Service, and Claims teams to training resources. The organization needed to provide a better experience to stakeholders and improve efficiency. After careful evaluation, Sentry selected a Whatfix digital adoption and experience layer to create a unique digital adoption experience for their end-users and stakeholders.
With Whatfix, Sentry Insurance is building personalized, in-app learning across critical insurance management and people applications. People can focus more time on new insurance sales opportunities, processing claims, and managing insurance policy inquiries.
The benefits included:
- Drove overall insurance business growth: In only 12 months, time-savings for content designers, developers, customers, and support staff totals more than $950,000 in resources, salaries, and re-gained productivity. Sentry can re-focus that value toward revenue-generating activities instead of the training content creation overhead.
- Reduced training content creation time by 40%: With Whatfix, it takes around 20 hours to create an item of content, compared to up to 50 hours previously. These time-savings add up rapidly – one Sentry application can have 500+ training content items.
- Delivered significant reduction in employee training time: Whatfix enables agents and other staff to use the applications without leveraging webinars or instructor-led sessions.
- Increased employee productivity: Sentry staff are proficient sooner in multiple customer and back office applications, working smarter in a hybrid work environment.
- Reduced policy and claims processing errors: Employees can easily catch policy and other mistakes with just-in-time nudges. Whatfix identifies and corrects errors inside the application with smart tips. Automated data input drastically reduces user errors.
Insurance Software & Technology Clicks Better With Whatfix
Accelerate your insurance digital transformation by enabling your employees and policyholders with contextual in-app guidance and constant real-time support with Whatfix’s digital adoption platform (DAP).
Whatfix empowers insurance IT teams with its no-code Visual Editor to create in-app, moment-of-need support and contextual guidance – all inside your insurance software applications and digital processes.
This reduces time-to-proficiency and achieves new levels of productivity and proficiency through better insurance technology adoption for all end-users, including customer-facing policyholders and internal employees across underwriters, claims agents, support staff, and more.
It also provides abilities for self-service, personalization, and guided user experiences for any application end-user – enabling end-users to use insurance technology, improving end-user productivity, and automating operations.
Whatfix empowers a data-driven approach by analyzing tech experiences with end-user behavioral analytics and event tracking. This identifies areas of friction in your insurance digital processes and tech experiences, allowing you to create optimal, contextual user journeys across various end-user segments.
With Whatfix, insurance IT teams can identify areas of friction causing issues and launch new in-app guided Flows, Smart Tips, and Self Help elements to guide and assist them with localized content that guides them through processes, driving workflow adoption and achieving business outcomes.
How does it work? Whatfix empowers enterprise insurance organizations to:
- Create in-app Flows and Task Lists that guide end-users step-by-step through digital processes and applications.
- Enable all end-users with Self Help, providing a searchable help wiki that connects to all your help and support documentation, FAQs, help desk articles, and more – that overlays on your applications’ digital UI.
- Notify end-users of process updates, compliance changes, team updates, deadlines, and more with Pop-Ups and Beacons.
- Provide contextual Smart Tips that give end-users timely information that nudges them to take the correct in-app action.
- Use Field Validation to ensure data is entered in full, in the correct format.
- Collect end-user feedback from end-users such as NPS, customer satisfaction surveys, staff training and onboarding feedback, and bug identification with In-App Surveys.
- Analyze end-user behavior with User Actions and Enterprise Insights by tracking custom in-app events to optimize user journeys, segment users into cohorts, identify areas of friction, and more.
With Whatfix, you can understand how your insurance technology is used and under-adopted by your employees, B2B customers, and end-user policyholders. This makes it easier to adjust software onboarding, training, support, and overall end-user adoption strategies—all to provide a seamless experience for every end-user that enables them with the right context and support to utilize new technologies and systems fully.